Table of Contents
Overview – Vision Testing
Vision testing is a core part of any neurological or ophthalmological examination, used to assess the functional integrity of the visual system. It includes visual acuity, eye movements, visual fields, colour discrimination, and pupillary reflexes. These tests can help identify refractive errors, retinal or optic nerve pathology, cranial nerve lesions, and other systemic conditions. This guide outlines the essential techniques and clinical significance of each vision test for medical students and OSCE preparation.
Visual Acuity Testing
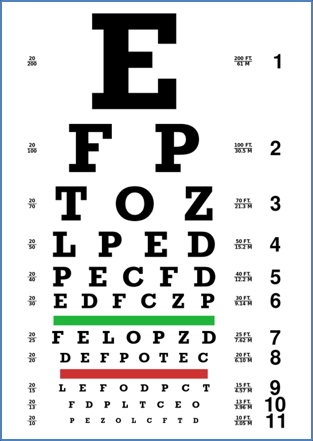
- Performed using a Snellen chart, typically at 6 metres (or standardised equivalent).
- Assesses corrected visual acuity (i.e. with glasses if usually worn).
- Each eye is tested individually, followed by both eyes together.
- Results are expressed as a fraction:
- Numerator = distance from chart (6m in Australia)
- Denominator = distance at which a person with normal vision could read the same line
- e.g. 6/12 means the patient can see at 6m what a person with normal vision sees at 12m
- Use a pinhole if acuity is reduced:
- If improves → refractive error
- No improvement → retinal/optic pathology
- If patient cannot read chart at all:
- Assess for:
- CF (Count Fingers)
- HM (Hand Movements)
- PL (Perception of Light)
- NPL (No Perception of Light)
- Assess for:
- For near vision: use a near-reading chart to assess presbyopia.
Extraocular Movements
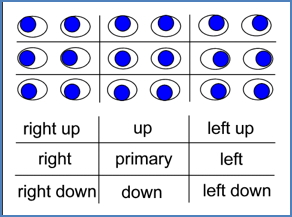
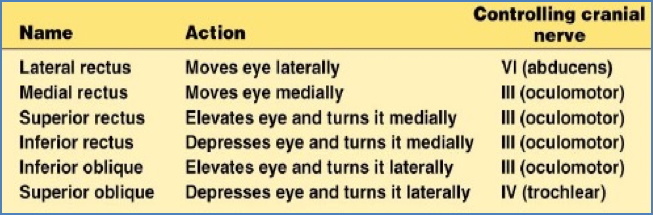
- Assesses cranial nerves III (oculomotor), IV (trochlear), and VI (abducens)
- Ask patient to follow a target in an ‘H’-shaped pattern, 6 inches in front of their face
- Check for:
- Conjugate gaze (eyes moving together)
- Nystagmus (involuntary eye oscillations)
- Strabismus or deviation
- Whether misalignment is comitant (same in all directions) or incomitant (varies)
- Convergence test: bring target close to nose and observe for pupillary constriction and medial eye movement
Visual Fields
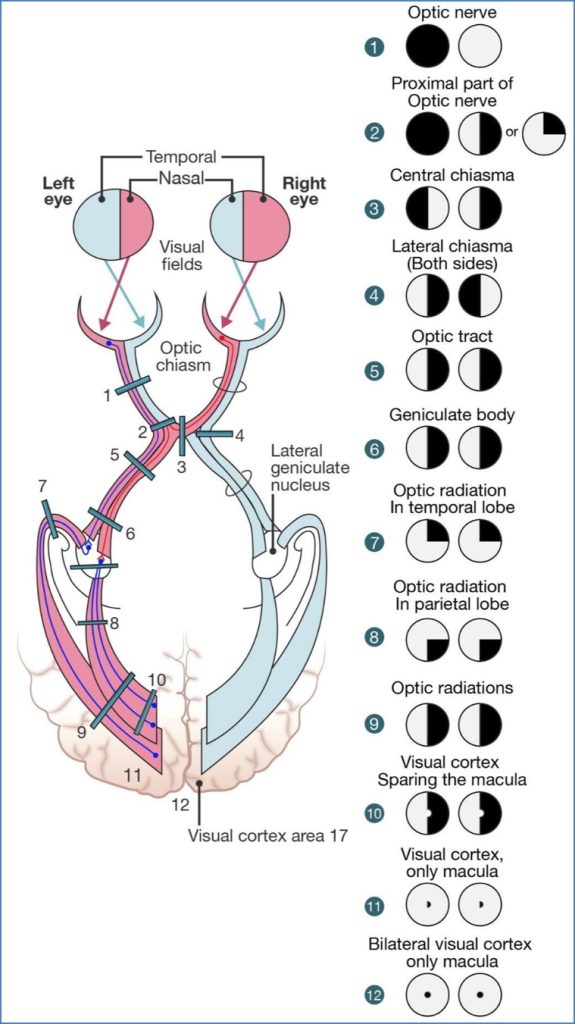
- Peripheral field testing:
- Sit opposite patient, both at eye level, arm’s length apart
- Cover your left eye; patient covers right eye and fixates on your eye
- Compare your visual field to theirs by moving your finger or red target from periphery inward
- Test all four quadrants per eye
- Remember: visual fields are inverted/reversed on the retina
- Upper field → inferior retina
- Temporal field → nasal retina
- Central field testing:
- Use an Amsler grid
- Patients with macular degeneration may report wavy or missing lines

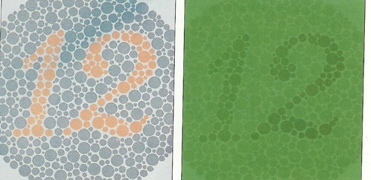
Colour Vision
- Use Ishihara plates
- Assesses cone photoreceptors, especially red-green discrimination
- Most colour blindness is X-linked recessive
- Affects ~8% of males, ~0.5% of females
- Red-green defects are most common
Pupillary Reflexes
- Mediated by the parasympathetic nervous system
- Assess both light response and accommodation
- PERLA = Pupils Equal, Round, Reactive to Light and Accommodation
Light Reflex
- Dim lights; ask patient to fixate on a distant target
- Shine a bright light in the right eye:
- Observe right pupil = direct response
- Observe left pupil = consensual response
- Repeat for the left eye
- Abnormality examples:
- If right pupil doesn’t constrict = right afferent OR efferent lesion
- If left pupil doesn’t constrict during consensual test = left efferent lesion

Accommodation Reflex
- Ask patient to look at a distant object, then at their own finger held ~8 inches from nose
- Look for:
- Pupillary constriction
- Eye convergence
- Used to test accommodation-mediated constriction
Special Notes
- Cataracts or corneal opacities may reduce light reflex in the affected eye
- Decreased stimulus to retina leads to weaker direct and consensual responses
Summary – Vision Testing
Vision testing encompasses a comprehensive suite of clinical assessments, including visual acuity, extraocular movement, field defects, colour vision, and pupillary responses. These tests are essential for diagnosing eye pathology and cranial nerve lesions, and they feature heavily in OSCEs and clinical practice. For a broader context, see our Clinical Skills Overview page.