Table of Contents
Overview – Male Genital Exam
The male genital exam is a routine yet vital component of clinical assessment in urology, sexual health, and general medicine. It encompasses inspection and palpation of the external genitalia and hernia screening, and may include a digital rectal exam to evaluate the prostate. The male genital exam plays a crucial role in identifying conditions such as testicular cancer, hernias, sexually transmitted infections (STIs), and prostate disease.
Preparation and Introduction
- Wash hands and introduce yourself to the patient
- Confirm the patient’s full name and age
- Explain the examination: involves inspection and palpation of the penis, testes, and hernia assessment
- Obtain informed consent
- Offer a gown or drape and provide privacy
- Ask the patient to stand (preferred for hernia inspection) or lie down if necessary
- Observe general appearance: comfort, distress, mobility
Examination of the Penis
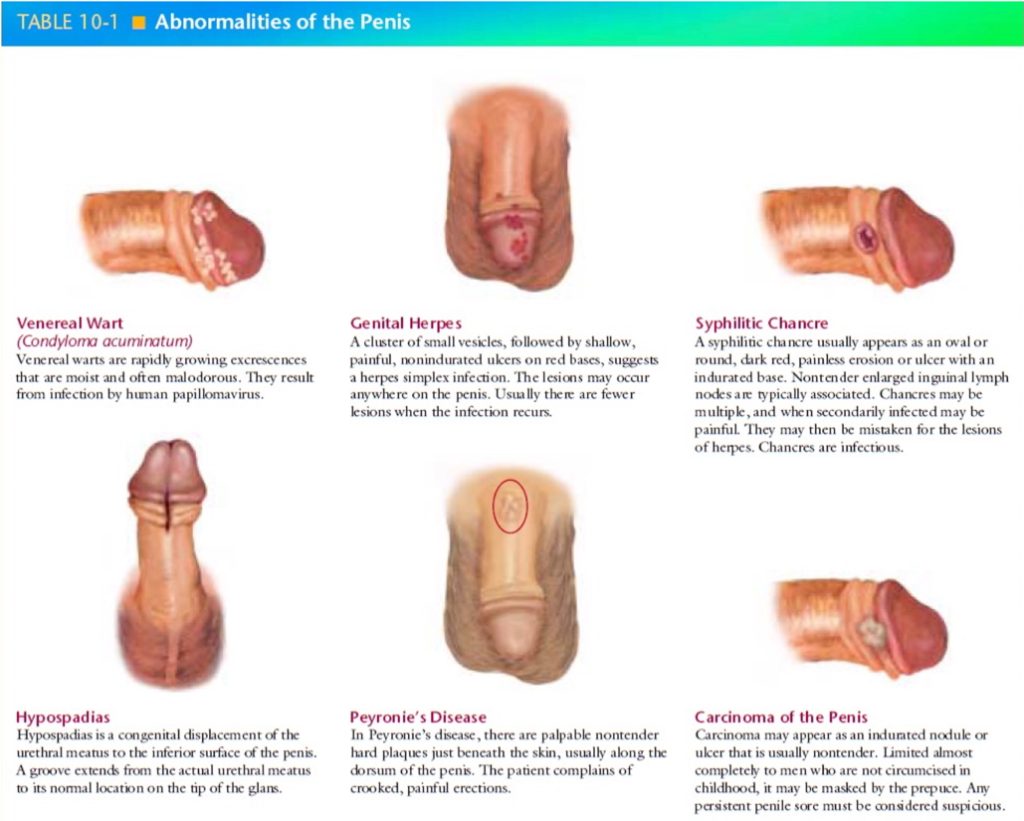
Inspection
- Glans:
- Note circumcision status
- Urethral meatus: check for hypospadias, discharge (ask patient to milk shaft)
- Retract foreskin: look for smegma, phimosis, paraphimosis
- Shaft:
- Inspect for lesions (vesicles, warts, ulcers), nodules, inflammation (e.g., balanitis)
- Palpate for tenderness, induration, or deformity
- Skin and Pubic Hair:
- Inspect base of penis for lice, burrows, excoriation
- Assess pubic hair distribution and hygiene
Examination of the Scrotum
Inspection
- Examine skin above, below, and behind the scrotum
- Identify rashes, lesions, epidermoid cysts
Palpation
- Testes and Epididymis:
- Assess size, consistency, shape, and presence of nodules
- Spermatic Cord:
- Palpate cord structures along the inguinal canal
- Masses:
- Transillumination test: cystic masses will transilluminate; solid masses will not


Hernia Assessment
Inguinal Hernias
- Inspection: Ask patient to bear down or cough
- Palpation:
- Use right index finger to examine right inguinal canal
- If hernia present, impulse felt at fingertip on coughing
- Auscultation: Bowel sounds may be audible in large hernias
Femoral Hernias
- Palpate near femoral artery
- Hernia typically appears just medial to the artery
- Ask patient to cough to provoke herniation
Health Promotion
- Recommend monthly testicular self-examination
- Advise cleaning beneath foreskin in uncircumcised men
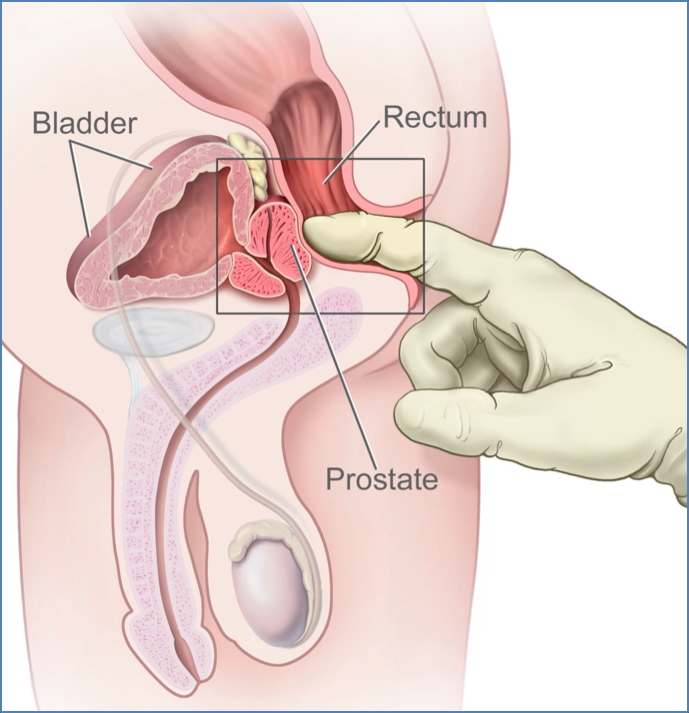
Digital Rectal and Prostate Examination
Patient Positioning
- Place patient in left lateral position with knees drawn up
- Ask them to move toward the edge of the bed until they contact your hip
Examination Steps
- Inspect perianal region: fissures, haemorrhoids, lesions, discharge
- Inform patient before beginning
- Lubricate index finger; place at anal verge and request patient to bear down
- Insert finger gently as sphincter relaxes
- Assess sphincter tone by asking patient to contract anus
Rectal and Prostate Palpation
- Perform 360° sweep for masses, tenderness, faeces
- Prostate assessment:
- Normal = smooth, rubbery with clear median sulcus
- Abnormal = nodular, firm, asymmetrical, obliterated sulcus, or tender (suggests prostatitis)
Completion
- Inform patient before removing finger
- Wipe finger on a towel and check for blood, pus, or mucus
- Gently clean patient’s anus and allow them to dress
Summary – Male Genital Exam
The male genital exam is a fundamental clinical skill encompassing inspection and palpation of the penis, testes, and groin, as well as a rectal exam for prostate assessment. It aids in detecting testicular cancer, sexually transmitted infections, hernias, and prostate abnormalities. For a broader context, see our Clinical Skills Overview page.