Table of Contents
Overview – Atherosclerosis
Atherosclerosis is a chronic, progressive inflammatory disease of large and medium-sized arteries, characterised by lipid accumulation, fibrosis, and plaque formation. It is the underlying cause of many cardiovascular diseases, including ischaemic heart disease, stroke, and peripheral vascular disease.
Terminology
- Athero- = Gruel/Fat (refers to lipid deposits in vessels)
- -sclerosis = Hardening (refers to fibrotic thickening of the arterial wall)
Lipid Review – The Key Players
Main Plasma Lipids:
- Cholesterol + Cholesterol Esters
- Phospholipids
- Triglycerides (Glycerol + Fatty Acids)
Lipid Transport Pathway:
- Dietary lipids absorbed in the small intestine
→ Packaged into chylomicrons
→ Enter lymphatics
→ Enter circulation via left subclavian vein
→ Travel to the liver
→ Liver repackages lipids into lipoproteins for systemic distribution
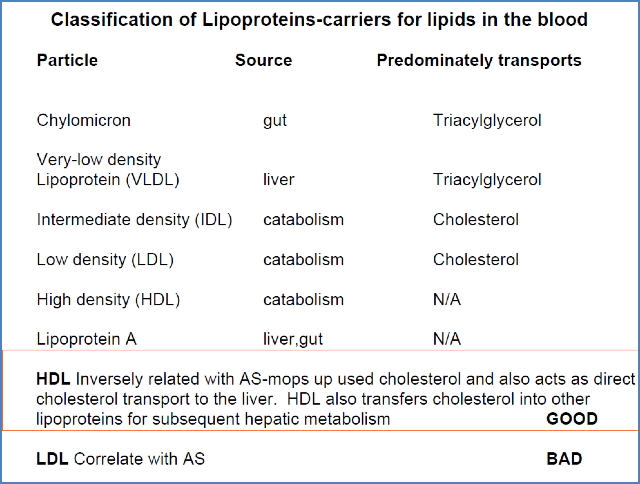
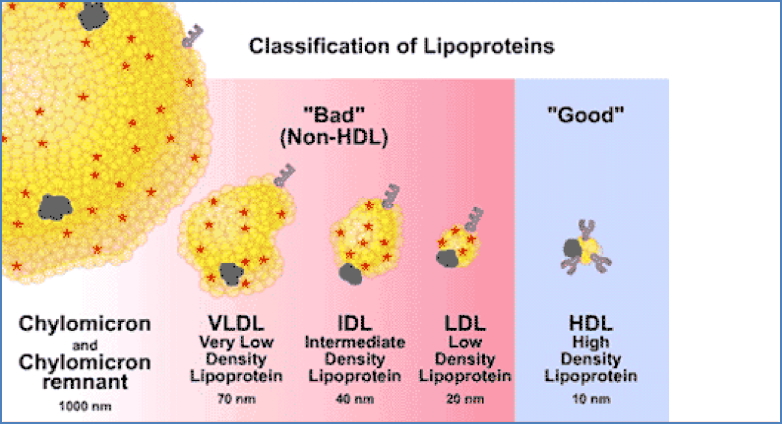
| Lipoprotein | Source | Function | Atherosclerosis Risk |
|---|---|---|---|
| LDL | Liver | Delivers cholesterol to tissues | Contributes to atheroma formation |
| HDL | Liver | Retrieves cholesterol from tissues → liver | Protective effect |
Aetiology
Key Contributing Factors
- Endothelial injury is the initiating event
- Strong inflammatory component
- A mix of non-modifiable and modifiable risk factors
Non-Modifiable
- Age (especially >40 years)
- Male sex
- Family history of cardiovascular disease
- Indigenous background
Modifiable
- Dyslipidaemia (↑LDL, ↓HDL)
- Hypertension
- Diabetes mellitus
- Smoking
- Obesity
- Metabolic syndrome
Pathogenesis – Step-by-Step
- 0. Endothelial Injury & Activation
- Triggers: Hypertension, Smoking, Diabetes, Oxidised LDL, Toxins, Infections
- Leads to endothelial dysfunction and increased permeability
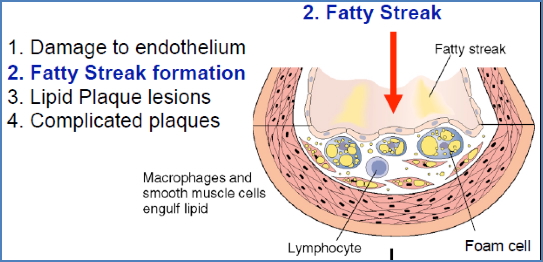
- 1. Endothelial Inflammation
- Recruitment of monocytes and smooth muscle cells into the intima
- Monocytes differentiate into macrophages

- 2. Lipid Accumulation – Fatty Streak Formation
- LDL infiltrates the vessel wall
- Macrophages engulf LDL → become foam cells
- Creates fatty streak under the tunica intima
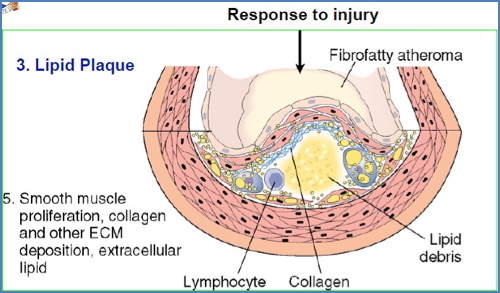
- 3. Plaque Growth – Atheroma Formation
- Foam cells die → release lipid debris
- Smooth muscle cells proliferate
- Cytokines and oxidised lipids promote connective tissue deposition
- Formation of a fibrous cap with a necrotic lipid core
- 4. Complicated Plaque – Rupture & Thrombosis
- Thin fibrous cap can rupture → exposes contents to blood
- Platelet activation → thrombus formation
- ↓ Perfusion = Clinical events (e.g., MI, stroke)


Clinical Features
Atherosclerosis affects multiple organ systems:
- Heart: Angina, myocardial infarction (MI)
- Brain: Ischaemic stroke
- Kidneys: Renal infarction
- Gastrointestinal tract: Mesenteric ischaemia
- Peripheral vessels: Claudication, gangrene, arterial ulcers
Investigations
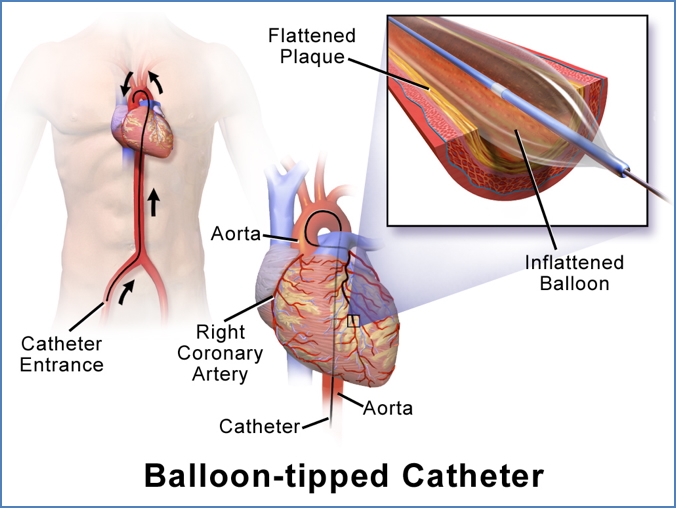
Invasive
- Coronary angiography via femoral artery
Non-Invasive
- CT coronary angiography (fast and accurate)
- May also use carotid Doppler, ankle-brachial index (ABI), or echocardiography depending on presentation
Management
1. Risk Factor Modification
- Statins for dyslipidaemia
- ACE inhibitors / β-blockers for hypertension
- Optimise glycaemic control in diabetes
- Lifestyle: weight loss, diet (low saturated fat), increased exercise
- Smoking and alcohol cessation
2. Thrombosis Prevention
3. Interventional
- Percutaneous coronary intervention (PCI) – balloon or stent
- Coronary artery bypass grafting (CABG) for severe cases


Complications
- Acute coronary syndrome (ACS)
- Thromboembolic stroke
- Renal impairment or infarction
- Critical limb ischaemia
- Sudden cardiac death
Summary – Atherosclerosis
Atherosclerosis is a progressive vascular pathology with major systemic consequences. It involves lipid accumulation, inflammation, and plaque formation, eventually leading to thrombosis and organ ischaemia. Early detection and risk factor modification—like statins, antihypertensives, and lifestyle changes—are vital. Explore more cardiovascular topics in our Cardiovascular Overview.