Table of Contents
Overview – Venous Thromboembolism
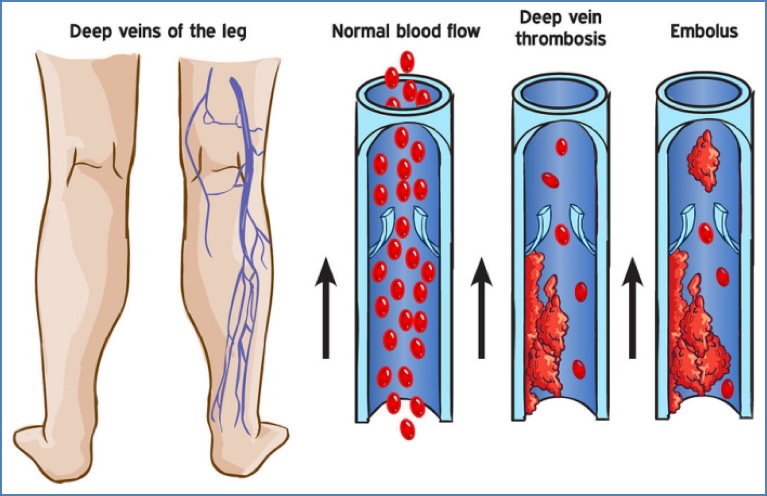
Venous thromboembolism encompasses Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE). It arises from thrombus formation in the deep veins, usually of the lower limbs, which can dislodge and embolise to the pulmonary arteries. Early diagnosis and management are essential to prevent life-threatening complications.
Definition
VTE = DVT (clot in deep venous system) ± PE (embolus travels to lungs).
It represents a spectrum of the same disease process driven by Virchow’s Triad:
1. Vessel wall injury
2. Venous stasis
3. Hypercoagulability
Virchow’s Triad
- Endothelial/Vessel Wall Injury
- Surgery
- Hypertension
- Smoking
- Stasis
- Prolonged immobility (e.g. long-haul flights, bed rest, post-operative)
- Congestive heart failure
- Obesity
- Pregnancy
- Hypercoagulability
- Malignancy (e.g. adenocarcinoma)
- Congenital disorders (e.g. antithrombin III deficiency, Factor V Leiden)
- Oestrogen therapies (e.g. oral contraceptive pill, hormone replacement therapy)
- Polycythaemia
Deep Vein Thrombosis (DVT)
Synonyms: Phlebothrombosis, Thrombophlebitis
Aetiology
- Venous valve incompetence
- Prolonged immobilisation (e.g. surgery, long-haul travel, bedrest)
- Risk factors = Virchow’s Triad:
- Vessel wall damage: surgery, smoking, hypertension
- Stasis: travel, obesity, pregnancy, CCF, post-operative states
- Hypercoagulability:
- Cancer (esp. adenocarcinoma)
- Congenital: Antithrombin III deficiency, Factor V Leiden
- Drugs: OCP, HRT
- Others: pregnancy, polycythaemia
Pathogenesis
Incompetent venous valves or immobility → ↓muscle pump → venous pooling → clot formation in deep leg veins (esp. calf)
Clinical Features
- Local symptoms (calf):
- Tenderness on palpation or passive dorsiflexion
- Redness, warmth, swelling
- Superficial venous dilation
- Distal oedema and cyanosis
- Complication:
- Pulmonary Embolism may be the first sign → sudden dyspnoea, chest pain, collapse
Investigations
- Duplex Doppler Ultrasound: 93% sensitivity, 98% specificity
Management
- Anticoagulation (oral DOAC or LMWH if contraindicated)
- +/- Thrombectomy
- +/- IVC filter if high PE risk or anticoagulation contraindicated

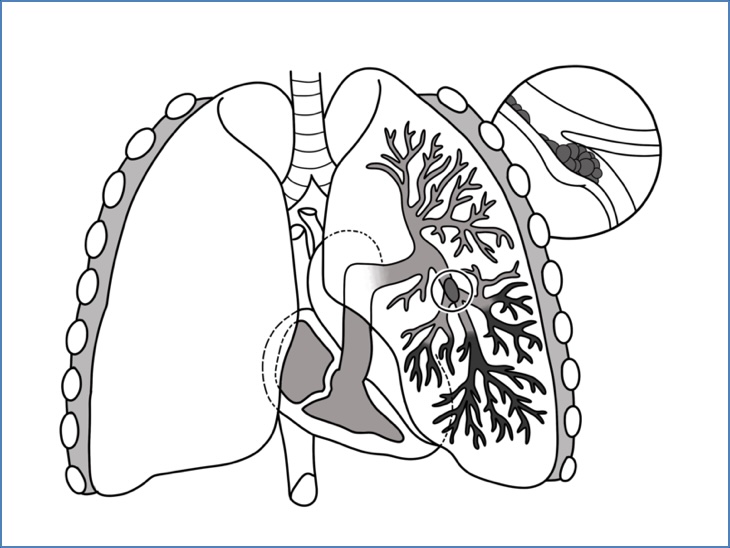
Pulmonary Embolism (PE)
Aetiology
- 95% originate from DVT (usually of lower limbs)
Pathogenesis
- DVT → thrombus embolises to pulmonary arteries →
- Ventilation-perfusion (V/Q) mismatch → respiratory failure
- Increased pulmonary vascular resistance → right heart strain → heart failure
Clinical Features
- Symptoms:
- Pleuritic chest pain ± pleural rub
- Dyspnoea, tachypnoea
- Cough ± haemoptysis
- +/- leg symptoms of DVT
- Signs:
- Right heart failure: raised JVP, tricuspid regurgitation
- Syncope, shock
- Fever
Investigations
- CT Pulmonary Angiogram (CTPA): gold standard – shows emboli in pulmonary arteries
- ECG: S1Q3T3 pattern
- V/Q scan: useful if CTPA contraindicated (e.g. renal impairment)
- CXR: later may show wedge-shaped infarct
Treatment
- Oxygen
- Anticoagulation (oral or heparin)
- Thrombolysis (TPA) if haemodynamic compromise
- +/- Surgical thrombectomy or IVC filter
Prevention
- Compression stockings
- Prophylactic anticoagulation
- IVC filter in severe risk or contraindication to anticoagulants

Summary – Venous Thromboembolism
Venous thromboembolism includes both deep vein thrombosis and pulmonary embolism, commonly resulting from stasis, hypercoagulability, and endothelial injury. Clinical presentation may be subtle or catastrophic, requiring a high index of suspicion. Prompt diagnosis via Doppler ultrasound or CT pulmonary angiography is essential, followed by appropriate anticoagulation and, where necessary, thrombolysis or thrombectomy. For a broader context, see our Cardiovascular Overview page.