Table of Contents
Overview – Physiology of Breathing
The physiology of breathing integrates ventilation, circulation, and gas exchange to maintain oxygen delivery and carbon dioxide removal. It involves both bronchial and pulmonary circulation, ventilation–perfusion matching, compliance of the lungs, and the energetic cost of ventilation. A solid understanding of breathing physiology is essential for interpreting respiratory diseases, exercise physiology, and conditions such as pulmonary embolism and pulmonary oedema.
Bronchial Circulation
- Provides O₂ and nutrient-rich blood to lung tissues.
- Originates from the systemic circulation via small bronchial arteries.
- Blood empties into pulmonary veins → left atrium.
- Note: Because of this, venous return to the left atrium is greater than right ventricular output.
Pulmonary Circulation
Features
- Much shorter than systemic circulation.
- Artery lumens are larger than systemic arteries due to:
- Thin walls (≈⅓ thickness of aorta).
- Distensible walls:
- Stretch to maintain low blood pressure.
- Prevent rupture of delicate pulmonary microvessels.
Pressures
- Pressures & resistance are much lower than systemic circuit → prevents microvessel rupture.
- Pulmonary artery:
- Systolic = 25 mmHg
- Diastolic = 8 mmHg
- Pulmonary capillary pressure: ≈ 7 mmHg
- Pulmonary vein: ≈ 2 mmHg
Resistance
- Much lower than systemic circulation.
- Extra-alveolar vessels → low resistance at high lung volumes (due to radial traction).
- At full lung volume:
- Transmural pressure overcomes radial traction.
- Vessel diameter decreases → resistance increases.
Blood Volume
- Average: 450–500 mL (≈9% of total blood volume).
- Only 70–100 mL participates in gas exchange at any moment.
- ≈70 mL replaced each heartbeat.
- Variability:
- Physiological:
- Blowing trumpet → ↑ thoracic pressure → may expel 250 mL blood.
- Acute blood loss → ↓ total volume → ↓ pulmonary blood volume.
- Posture: standing ↓ pulmonary volume by ≈10%.
- ↑ Systemic vascular tone → squeezes blood into pulmonary circuit.
- Pathological:
- Left heart failure → blood backs up → ↑ pulmonary blood volume.
- Physiological:
Blood Flow
- Pulmonary blood flow = cardiac output.
- Anything affecting CO (HR, SV, contractility, venous return) equally affects pulmonary flow.
Hypoxic Vasoconstriction (PO₂ vs. Blood Flow)
- Pulmonary blood flow is directed to the best-ventilated alveoli.
- Opposite of systemic circulation.
- If PAO₂ (alveolar partial pressure of O₂) falls:
- Adjacent vessels constrict → restricts blood flow to poorly ventilated alveoli.
- Acts as an automatic mechanism to match ventilation with perfusion.
Regional Pulmonary Blood Flow
Ventilation-Perfusion Matching
- Not all alveoli are ventilated or perfused equally.
- Even in healthy lungs → some mismatch occurs.
- Quantified as the ventilation-perfusion ratio (V̇A/Q̇).
- Blood flow and ventilation both increase toward the base of the lung (flow > ventilation).
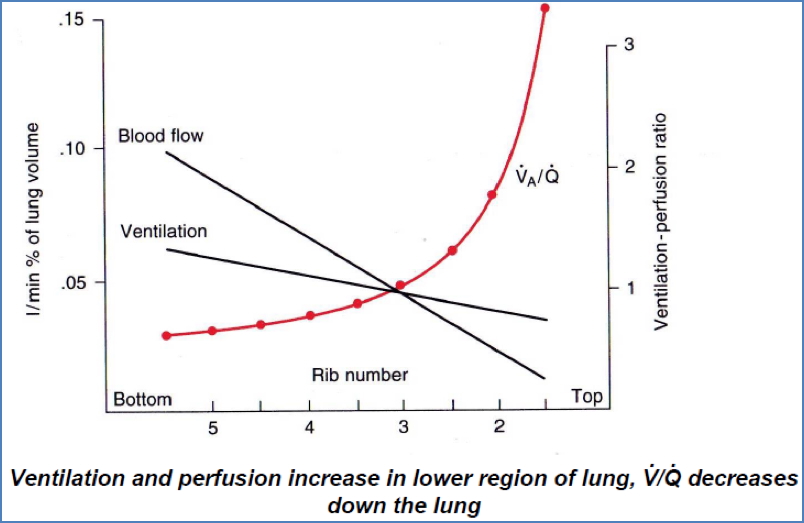
V/Q Ratios
- V̇A/Q̇ = Alveolar ventilation rate / Blood flow rate.
- Approaching zero:
- Ventilation = 0, but perfusion present.
- Alveolar gas partial pressures equilibrate with venous blood.
- Approaching infinity:
- Ventilation present, but no perfusion.
- Alveolar gases equilibrate with atmosphere.

Effect of Gravity
- Arterial pressure (Pa):
- Lower at lung apex.
- Higher at base.
- Pressure difference ≈ 23 mmHg.
- Standing: little flow at apex, ≈5× flow at base.

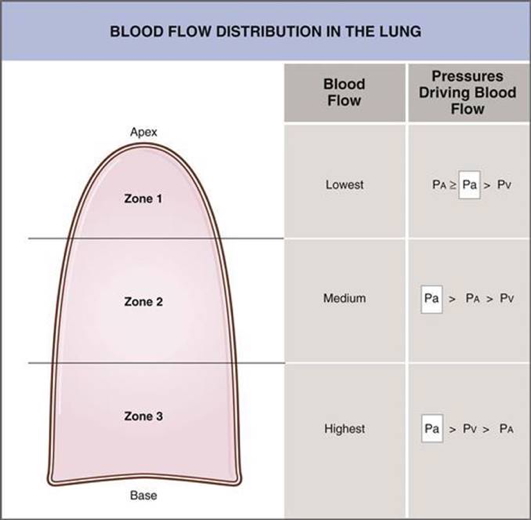
Transmural Pressure (Blood vs. Alveolar Air Pressure)
- Capillaries distended by internal blood pressure.
- Compressed by alveolar air pressure.
- Net effect determines perfusion (vessel patency).
- West’s Zones of the Lung:
- Zone 1:
- Alveolar pressure > capillary pressure.
- No blood flow.
- V/Q → ∞
- (Abnormal condition).
- Zone 2:
- Capillary pressure > alveolar pressure only in systole.
- Intermittent blood flow.
- V/Q ≈ normal.
- Zone 3:
- Capillary pressure always > alveolar pressure.
- Continuous flow.
- V/Q still normal but lower.
- Zone 1:
- Normal lung: mostly Zone 2 & 3.
Effect of Exercise on Pulmonary Blood Flow
- Pulmonary blood flow ↑ 4–7×.
- Pulmonary BP rise must remain low to prevent microvessel rupture.
- Adaptations:
- Capillary distension.
- Recruitment of previously closed capillaries.
- Mild ↑ pulmonary arterial pressure.
Pulmonary Capillaries
Dynamics
- Normal capillary transit time: ≈ 0.8 sec.
- During exercise: shortened to ≈ 0.3 sec.
- If <0.3 sec → inadequate gas exchange.
Fluid Exchange
- Governed by same forces as systemic capillaries:
- Hydrostatic pressure.
- Colloid-osmotic pressure.
- Magnitudes differ:
- Hydrostatic pressure ≈ 7 mmHg (lower than systemic).
- Interstitial hydrostatic pressure slightly negative → keeps alveoli “dry”.
- Colloid-osmotic pressure ≈ –28 mmHg → draws fluid back into capillaries, opposes hydrostatic pressure.
- Pulmonary capillaries are relatively leaky to proteins:
- Some proteins enter interstitium.
- Interstitial osmotic > alveolar osmotic pressure.
- Draws fluid from alveoli → interstitium → prevents alveolar flooding.
- If too leaky → proteins accumulate → pulmonary oedema.

Preventing Pulmonary Oedema
- Negative interstitial pressure:
- Keeps alveoli dry.
- Draws alveolar fluid into interstitium → lymphatics.
- If interstitial pressure becomes positive → oedema occurs.
- Lymphatics:
- Drain interstitial fluid back to blood.
- Oedema Safety Factor:
- Pulmonary capillary pressure ≈ 7 mmHg.
- Plasma colloid osmotic pressure ≈ –28 mmHg.
- Capillary pressure must ↑ >21 mmHg to overcome → risk of lethal oedema.
- Chronic pressure rise → lymph vessel adaptation.

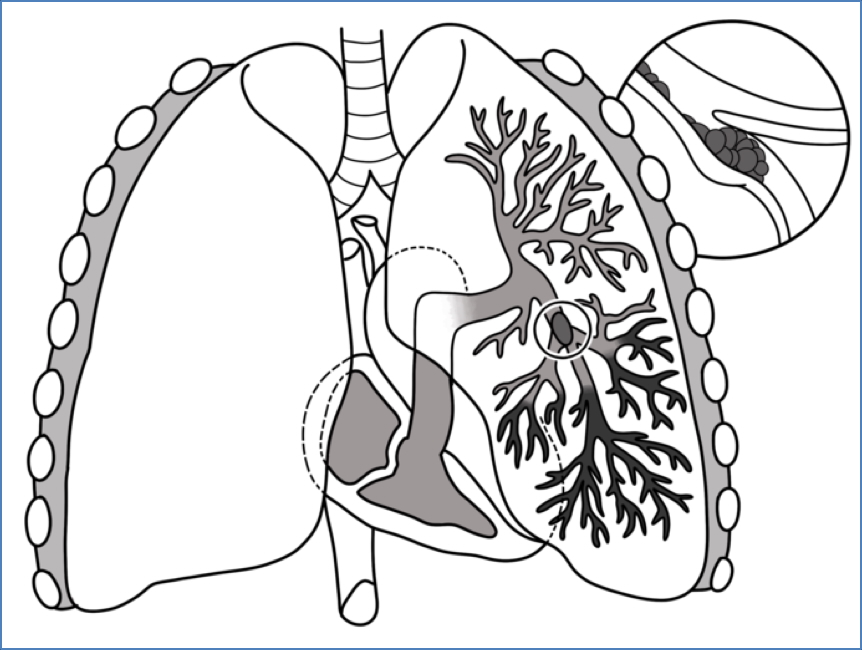
Pulmonary Embolism
- Foreign material obstructing a pulmonary vessel.
- Most commonly blood clot (thrombus).
- Prevents oxygenation of blood in affected region.
Pulmonary Ventilation (Breathing)
- Definition: physical movement of air into/out of respiratory tract.
- Distinct from respiration.
- Aim: maintain adequate alveolar ventilation.
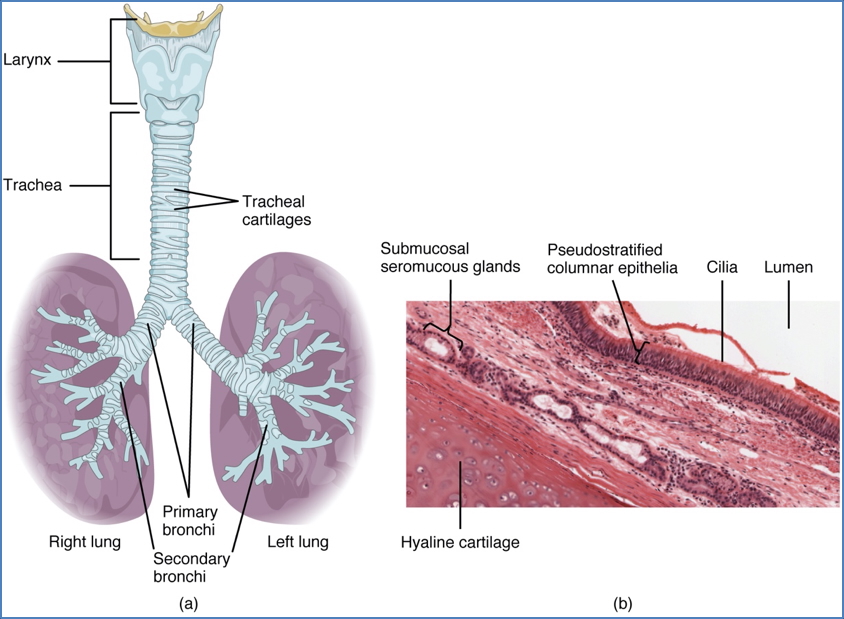
Conducting Zone
- No gas exchange.
- Moves air → alveoli.
- Filters particulates.
- Structures:
- Nose, mouth, nasopharynx.
- Trachea.
- Bronchi.
- Bronchioles.
- Patency maintained by:
- Cartilage rings (trachea).
- Cartilage plates (bronchi).
- Transmural pressure + radial traction (bronchioles).
- Patency problems:
- Snoring.
- Sleep apnoea.
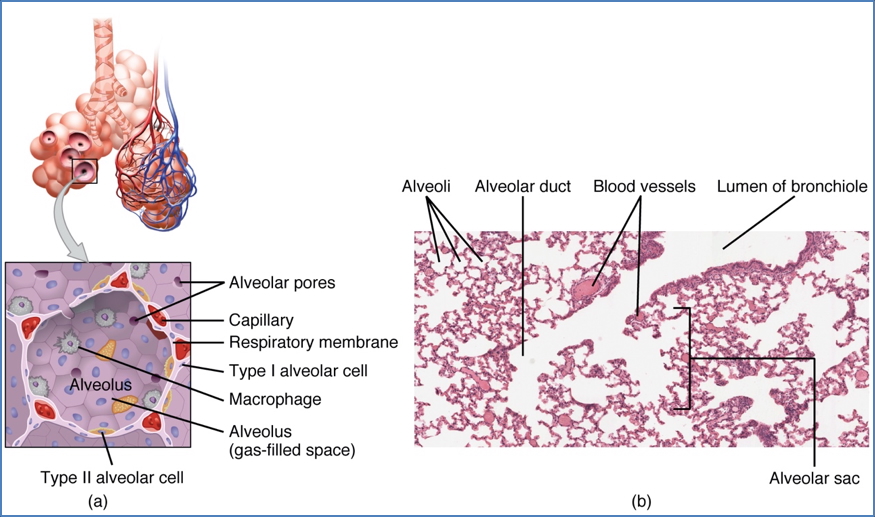
Respiratory Zone
- Site of gas exchange.
- Structures: respiratory bronchioles, alveolar ducts, alveoli.
- Rich blood supply.
- Patency maintained by:
- Negative intrapleural pressure.
- Alveolar surface tension.
- Patency problems:
- Emphysema.
- Asthma.
- Infant respiratory distress syndrome.
Lung Compliance
- Ease of lung expansion.
- Defined as: pressure change required to produce volume change.
- Low compliance = lungs stiff → greater force needed.
- Influencing factors:
- Pulmonary connective tissue: ↑ fibrosis → ↓ compliance.
- Surfactant: ↓ surfactant → ↓ compliance.
- Thoracic cage mobility: ↓ mobility (arthritis, scoliosis) → ↓ compliance.
Energetic Cost of Ventilation
- Resting ventilation = 3–5% of body’s energy demands.
- Cost increases with:
- ↑ Tidal volume (exercise).
- ↓ Compliance (↓ surfactant, ↑ fibrosis, ↓ thoracic mobility).
- ↑ Airway resistance (bronchoconstriction: asthma, emphysema).
- Airway diameter = extremely powerful determinant of flow rate.
- In some diseases, cost of breathing is so high that respiratory muscles consume more O₂ than they deliver.

Summary – Physiology of Breathing
The physiology of breathing involves bronchial and pulmonary circulation, ventilation–perfusion matching, lung compliance, and the mechanics of pulmonary blood flow. Protective mechanisms prevent pulmonary oedema, while ventilation ensures adequate alveolar gas exchange. Pathological states such as embolism, fibrosis, and asthma disrupt these processes. For a broader context, see our Respiratory Overview page.