Table of Contents
Overview – Brain Tumours
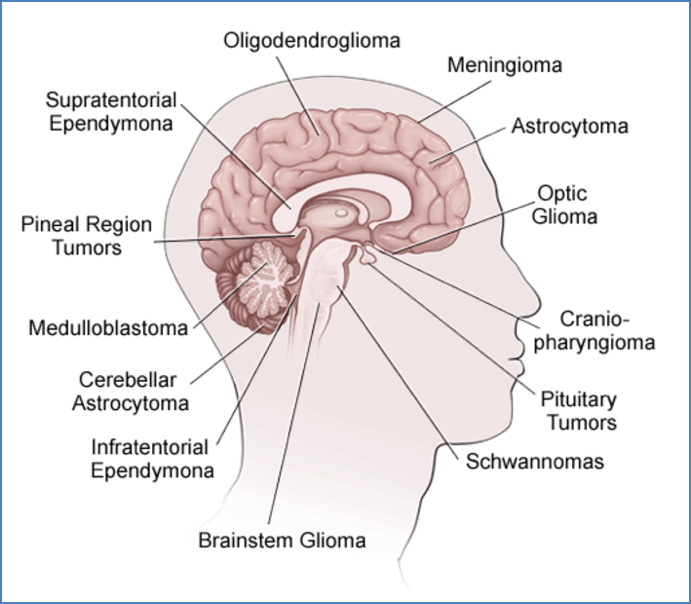
Brain tumours are a diverse group of neoplasms affecting the central nervous system (CNS), with varying origins, locations, and behaviours. In adults, tumours are predominantly supratentorial (cerebral), while in children they are mostly infratentorial (cerebellum and brainstem). Importantly, CNS tumours never metastasise outside the CNS, though some may spread via CSF pathways. This article outlines the key tumour types, clinical features, and management strategies relevant to final-year medical students.
General Features
- Adults: Most tumours are cerebral/supratentorial
- Children: Most tumours are infratentorial (e.g. cerebellum, brainstem)
- Metastases:
- Often secondary to lung, breast, GIT, melanoma
- Primary tumours: Most commonly gliomas (not neuronal in origin)
- Key note: CNS tumours do not metastasise outside the CNS


Clinical Features
- General signs:
- Chronic, crescendo morning headache
- Vomiting, papilloedema, seizures
- Progressive neurological deficits (focal signs depend on location)
- Location-specific signs:
- Frontal lobe → personality changes, disinhibition
- Temporal lobe → language, hearing deficits
- Occipital lobe → visual field defects
- Motor cortex → limb weakness
- Cerebellum → ataxia, gait disturbance
- Brainstem → cranial nerve palsies, obtundation

Primary CNS Tumours
Adult Tumours
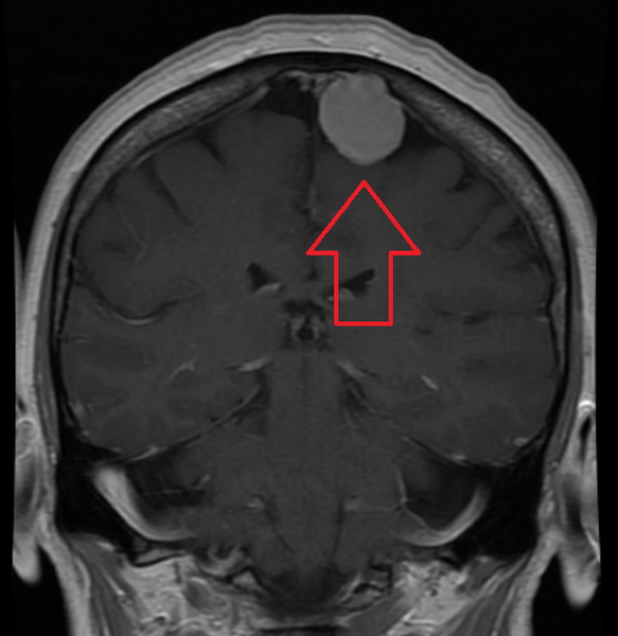
1. Meningioma
- Origin: Arachnoid cap cells
- Macro: Dura-attached, well-circumscribed, calcified
- Features:
- Benign and slow-growing
- Compression of adjacent brain tissue
- Headache, often worse during pregnancy
- Treatment: Surgical resection
- Prognosis: Excellent
2. Low-Grade Astrocytoma
- Origin: Astrocytes
- Macro: Solid, supratentorial mass
- Features:
- Headache, personality change, focal neurology
- Treatment: Surgical excision
- Prognosis: Good (90% 5-year survival)

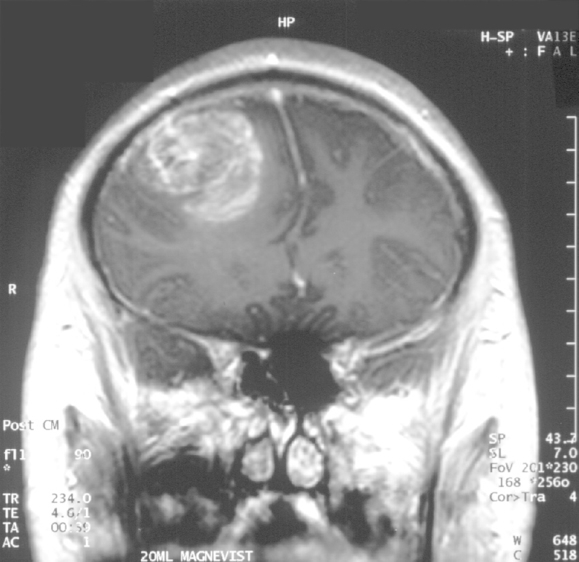
3. Glioblastoma Multiforme (GBM)
- Origin: High-grade astrocyte tumour
- Macro: Supratentorial, solid with possible cysts
- Features:
- Rapid progression, severe headache, seizures
- Personality changes, hemiparesis
- Treatment: Palliative (surgery + chemo/radiotherapy + corticosteroids)
- Prognosis: Poor (<1 year median survival)
Childhood Tumours
1. Pilocytic Astrocytoma
- Location: Cerebellum
- Macro: Cystic, well-demarcated
- Features:
- Ataxia, nystagmus, failure to thrive
- Associated with Neurofibromatosis type 1
- Treatment: Surgical resection
- Prognosis: Excellent (>90% 10-year survival)
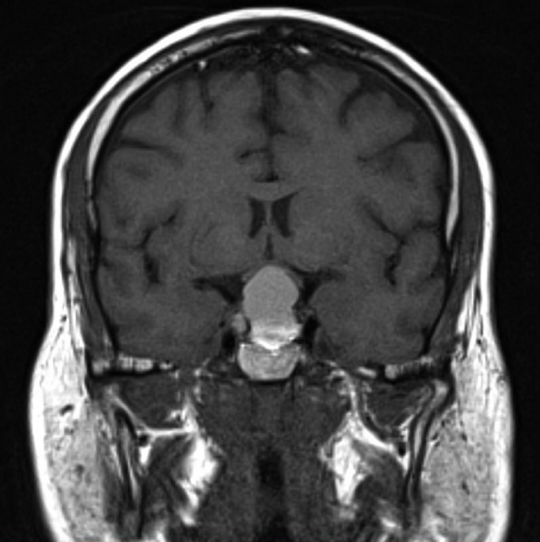
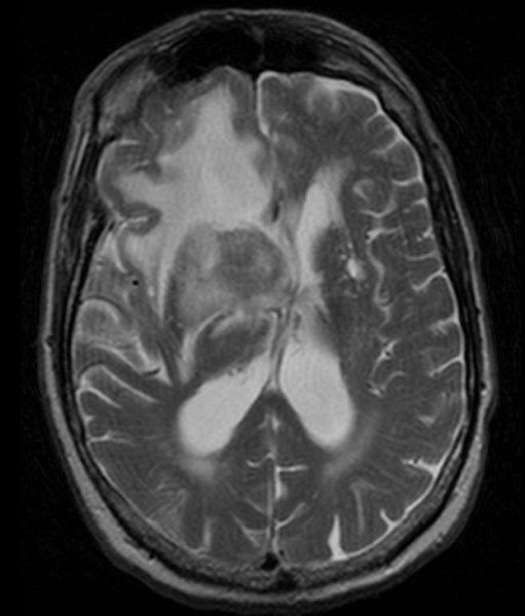
2. Medulloblastoma
- Origin: Neuroectodermal (germ cell-derived)
- Location: 4th ventricle, cerebellum
- Features:
- Obstructive hydrocephalus: morning headache, vomiting
- Gait instability, diplopia, cerebellar signs
- Treatment: Surgical resection + radiation + chemotherapy
- Prognosis: Poor (70% 5-year survival; CSF spread common)

Other CNS Tumours
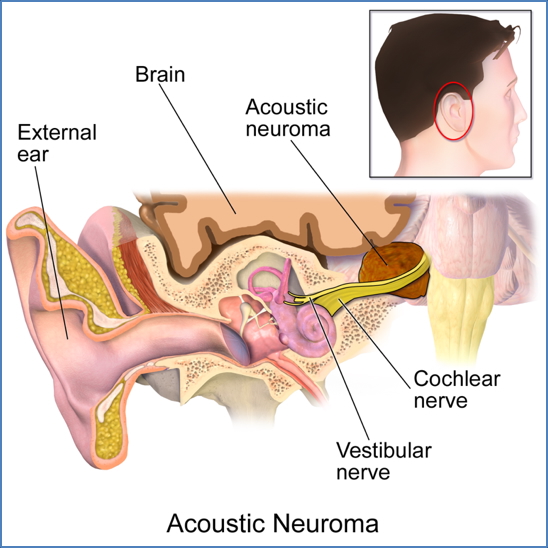
Acoustic Neuroma (Vestibular Schwannoma)
- Origin: Schwann cells of CN VIII
- Features:
- Typically 50-60yrs old
- Benign; slow-growing
- Tinnitus, hearing loss, vertigo
- Cerebellopontine Syndrome: Cranial nerve deficits (V, VII, IX, X) if large
- CN 5 (Trigeminal) Palsy: Ipsilateral ↓Corneal Reflex, Trigeminal Neuralgia, ↓Sensation
- CN 6 (Abducens) Palsy: Diplopia, Ipsilateral Inward-Facing Eye
- CN 7 (Facial) Palsy: Ipsilateral Facial Weakness
- (CN 8 (V/C): Ipsilateral Deafness, Tinnitus, Vertigo)
- Ipsilateral Cerebellar Signs: Nystagmus, Ataxia
- Treatment: Surgery or radiosurgery
- Prognosis: Excellent, though facial nerve injury risk exists
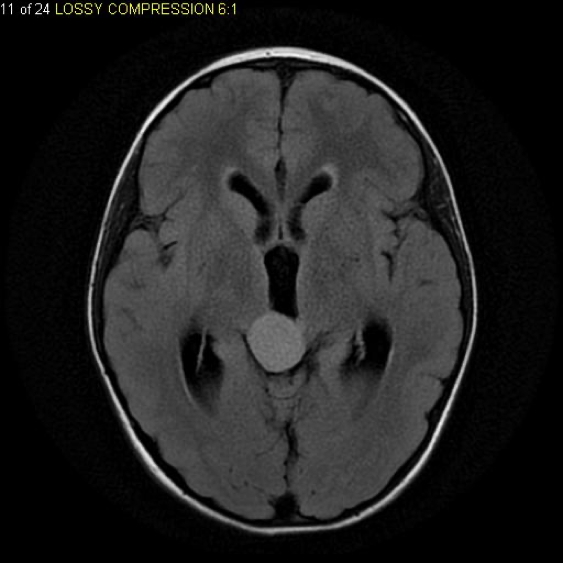
Pituitary Adenoma
- Origin: Anterior pituitary cells
- Features:
- Headache
- Bitemporal hemianopsia (optic chiasm compression)
- Hypopituitarism or hormone hypersecretion
- Treatment: Trans-sphenoidal surgery + hormone therapy
- Prognosis: Good, but recurrence common
Neurofibromatosis (Type 1 & 2)
- Origin: Neural fibroblasts
- Features:
- Benign
- Multiple neurofibromas
- NF1 – Familial & Sporadic
- NF2 – Autosomal Dominant
- NF2: Bilateral acoustic neuromas + juvenile cataracts
- Treatment: Surgical excision
- Prognosis: Benign but can cause severe disfigurement

CNS Lymphoma
- Origin: B-cell lymphoma (often EBV-associated in immunosuppressed)
- Features:
- Malignant
- Headache, seizures, focal deficits, constitutional B-symptoms (Fever, Night Sweats, Weight Loss)
- Treatment: Chemotherapy + steroids (surgery not feasible)
- Prognosis: Poor (median survival ~10 months)
Summary – Brain Tumours
Brain tumours differ between adults and children in location and type. Adults typically present with supratentorial tumours (e.g. meningiomas, glioblastomas), while children present with infratentorial tumours (e.g. pilocytic astrocytoma, medulloblastoma). Presentations vary depending on location and tumour growth. Timely imaging, surgical intervention, and adjuvant therapies are critical for management. For a broader context, see our Nervous System Overview page.