Table of Contents
Overview – Benign Skin Cysts
Benign skin cysts are common subcutaneous lesions that present across various age groups and anatomical sites. While usually asymptomatic, they may cause cosmetic concern, inflammation, or secondary infection. Final-year medical students should understand the distinguishing features of different benign cyst types, their pathophysiology, and when intervention is appropriate. This guide to benign skin cysts covers the clinical features and management of epidermal, pilar, ganglion cysts, and milia.
Epidermal Cyst
Clinical Features
- Round, firm, mobile nodule
- Slow-growing; 1–several cm in diameter
- May have a central punctum (enlarged pore)
- Often located on face, neck, back, or trunk
Pathophysiology
- Involves the cystic enclosure of epidermal cells within the dermis
- Fills with keratin and lipid-rich debris (cream-coloured, odorous)
- Thin cyst wall → prone to rupture → inflammation and tenderness
Epidemiology
- Most common type of skin cyst
- Typically affects young to middle-aged individuals
Clinical Course
- May rupture and become painful or inflamed
- Can increase in size or number with time
Management
- Usually self-limiting
- Excision may be required if inflamed, infected, or cosmetically concerning


Pilar Cyst (Trichilemmal Cyst)
Clinical Features
- Smooth, firm, dome-shaped nodules
- Size: 0.5–5 cm
- Lacks central punctum
- 90% occur on the scalp
Pathophysiology
- Arises from the outer root sheath of hair follicles
- Cyst contents are dense keratin
- May calcify
- Pressure can cause atrophy of overlying hair follicles
Epidemiology
- Second most common skin cyst
- Common in middle-aged females
Clinical Course
- May rupture → inflammation and discomfort
Management
- Surgical excision (often removed intact)

Ganglion Cyst
Clinical Features
- Solitary, rubbery swelling
- Usually adjacent to a joint or tendon sheath
- Common on the wrist or hand
Pathophysiology
- Arises from synovial fluid herniation
- Often associated with osteoarthritis or joint degeneration
Epidemiology
- More frequent in older adults
Clinical Course
- Often stable
- May limit joint mobility
Management
- Observation unless symptomatic
- Aspiration or surgical removal in select cases

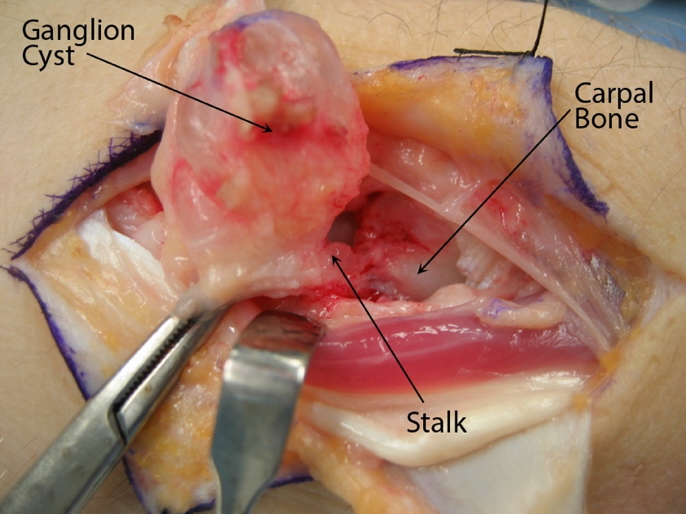
2. Credit: https://orthoinfo.aaos.org/
Milia
Clinical Features
- 1–2 mm pearly white or yellowish papules
- Commonly located on eyelids, cheeks, and forehead
- Superficial and non-inflammatory
Pathophysiology
- Epidermoid keratin accumulation under the stratum corneum
- Can occur spontaneously or after skin trauma (burns, dermabrasion, radiation)
- May be associated with blistering dermatoses (e.g. epidermolysis bullosa, porphyria cutanea tarda)
Epidemiology
- Very common in neonates (physiological milia)
- Can occur at any age
Clinical Course
- Self-resolves in ~4 weeks in newborns
Management
- Typically no treatment needed
- Contents can be expressed manually for cosmetic reasons

Summary – Benign Skin Cysts
Benign skin cysts include a spectrum of lesions such as epidermal, pilar, ganglion cysts, and milia, each with distinct clinical and pathological features. Most are harmless and self-limiting, though some may require excision if symptomatic. Recognising the morphology and progression of benign skin cysts helps guide appropriate management and patient reassurance. For a broader context, see our Skin & Dermatology Overview page.