Table of Contents
Overview – Hyperthyroidism
Hyperthyroidism refers to excessive secretion of thyroid hormones, leading to widespread hypermetabolic effects across multiple organ systems. Graves’ disease remains the most common cause globally, with other causes including toxic multinodular goitre and subacute thyroiditis. Prompt diagnosis and treatment are essential to prevent severe complications such as thyrotoxic storm.
Definition
- Hyperthyroidism: Excess thyroid hormone secretion (T3, T4) causing increased basal metabolic rate and sympathetic activity.
Aetiology
Autoimmune
- Graves’ disease:
- Thyroid-stimulating antibodies (TsAb) mimic TSH.
- Stimulate T3/T4 overproduction.
Nodular
- Toxic multinodular goitre:
- Autonomous thyroid nodules develop within a pre-existing goitre.
- Independently secrete thyroid hormones.
Subacute Thyroiditis
- Post-URTI Subacute (“De-Quervain’s”) Thyroiditis:
- Transient hyperthyroid phase followed by hypothyroid or euthyroid state.
Pathophysiology
- ↑ Basal metabolic rate
- ↑ Sympathetic sensitivity
- ↑ Thermogenesis → Heat intolerance
- If Graves’ disease: characteristic exophthalmos and goitre
Clinical Features
General
- Fatigue
- Heat intolerance
Cardiovascular
- Tachycardia
- Palpitations
- Atrial fibrillation (particularly in elderly)
- Cardiomegaly
- Congestive heart failure
Gastrointestinal
- Weight loss despite increased appetite
- Thirst
- Increased bowel frequency, diarrhoea
Neurological
- Sympathetic overactivity:
- Fine tremor
- Irritability, anxiety, insomnia
- Proximal myopathy and muscle wasting
Ocular
Dermatological
- Acropachy (digital clubbing, swelling of fingers and toes)
- Fine hair, alopecia
- Warm, flushed, sweaty skin
- Vitiligo
- Plummer’s nails (onycholysis)
Musculoskeletal
- Increased bone resorption → Osteoporosis
Haematological
- Lymphadenopathy (especially in Graves’)
Other
- Menorrhagia
- Pretibial myxoedema

Investigations
- TSH: suppressed
- T3/T4: elevated
- Autoimmune screening (Graves):
- Thyroid-stimulating immunoglobulins (TSI/TsAb)
Management
Medical
- Anti-thyroid drugs:
- Carbimazole (first-line)
- Propylthiouracil (alternative, especially in pregnancy)
Radioactive Iodine Therapy
- Iodine-125 to destroy thyroid tissue.
- Risk of inducing hypothyroidism.
Surgical
- Partial or total thyroidectomy.
- Used for refractory cases, large goitres, or compressive symptoms.
Complications
Thyrotoxic Storm (Thyroid Crisis)
- Life-threatening hyperthyroid emergency with ~50% mortality if untreated.
Triggers
- Infection, trauma, surgery, myocardial infarction, heart failure.
Clinical Features
- Extreme fever
- Severe tachycardia and arrhythmias
- Hypotension, vascular collapse
- Heart failure, pulmonary oedema
- Vomiting, diarrhoea
- Confusion, delirium, coma
Differentials
- Sepsis
- Phaeochromocytoma
- Malignant hyperthermia
Laboratory Findings
- Markedly ↑ T3/T4
- Markedly ↓ TSH
- Leukocytosis
- Hypercalcaemia
- Elevated liver enzymes
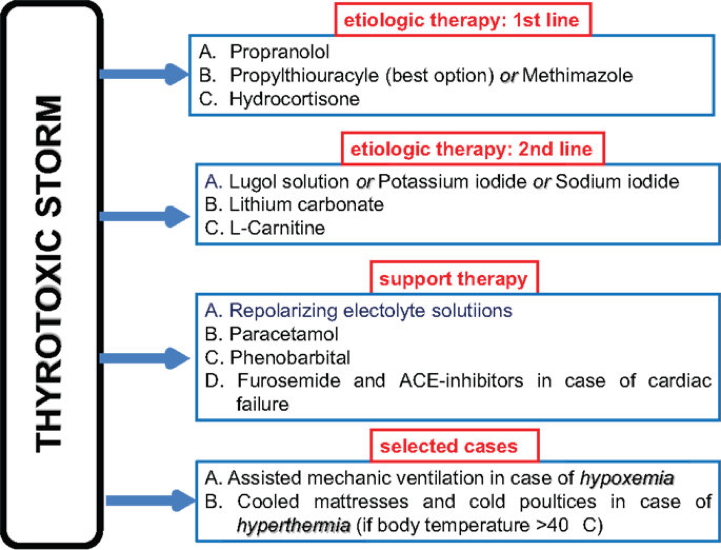
Management
- Treat precipitating cause.
- Supportive care (ABCs, fluid resuscitation, cooling measures).
- Beta-blockers (propranolol) to control sympathetic symptoms.
- Antithyroid medications (high-dose carbimazole or propylthiouracil).
- Steroids (hydrocortisone) to reduce conversion of T4 to T3.
- Iodine solution (Lugol’s iodine) in select cases after antithyroid pretreatment.
Summary – Hyperthyroidism
Hyperthyroidism describes excess secretion of thyroid hormones, most commonly due to Graves’ disease. It causes multi-system hypermetabolic symptoms and can progress to life-threatening thyrotoxic storm if not promptly managed. For a broader context, see our Endocrine Overview page.