Table of Contents
Overview – Gastroenteritis
Gastroenteritis is a common clinical syndrome characterised by inflammation of the stomach and intestines, typically resulting in diarrhoea and vomiting. It may be viral, bacterial, or parasitic in origin and is a key cause of global morbidity, especially in children and travellers. While often self-limiting, some forms—such as dysenteric or toxigenic infections—require specific intervention. This article covers the key causative organisms, clinical features, and management principles for gastroenteritis.
Definition
Gastroenteritis refers to inflammation of the gastrointestinal tract—mainly the stomach and intestines—resulting in vomiting, diarrhoea, abdominal cramps, and fever.
Aetiology
Bacterial Causes
- Toxigenic Diarrhoea (Food Poisoning)
- Staphylococcus aureus – linked to poor food handling
- Bacillus cereus – found in cereals and rice
- Incubation period: <4 hours
- Escherichia coli (E. coli)
- ETEC – Enterotoxigenic: Traveller’s diarrhoea
- EIEC – Enteroinvasive: Dysentery
- EPEC – Enteropathogenic: Infant diarrhoea
- EHEC – Enterohaemorrhagic: Produces verotoxin → Haemolytic-Uraemic Syndrome (HUS):
- → Kidney failure, thrombocytopaenia, bloody diarrhoea
- Salmonella typhi (Typhoid Fever)
- Causes dysentery and systemic symptoms: Rose spots, delirium, fever, bowel perforation
- Listeria monocytogenes
- Associated with soft cheese, cold deli meats
- Risk: Pregnant women and immunocompromised
- Vibrio cholerae (Cholera)
- Profuse, rice-water stools
- Often self-limiting with supportive care

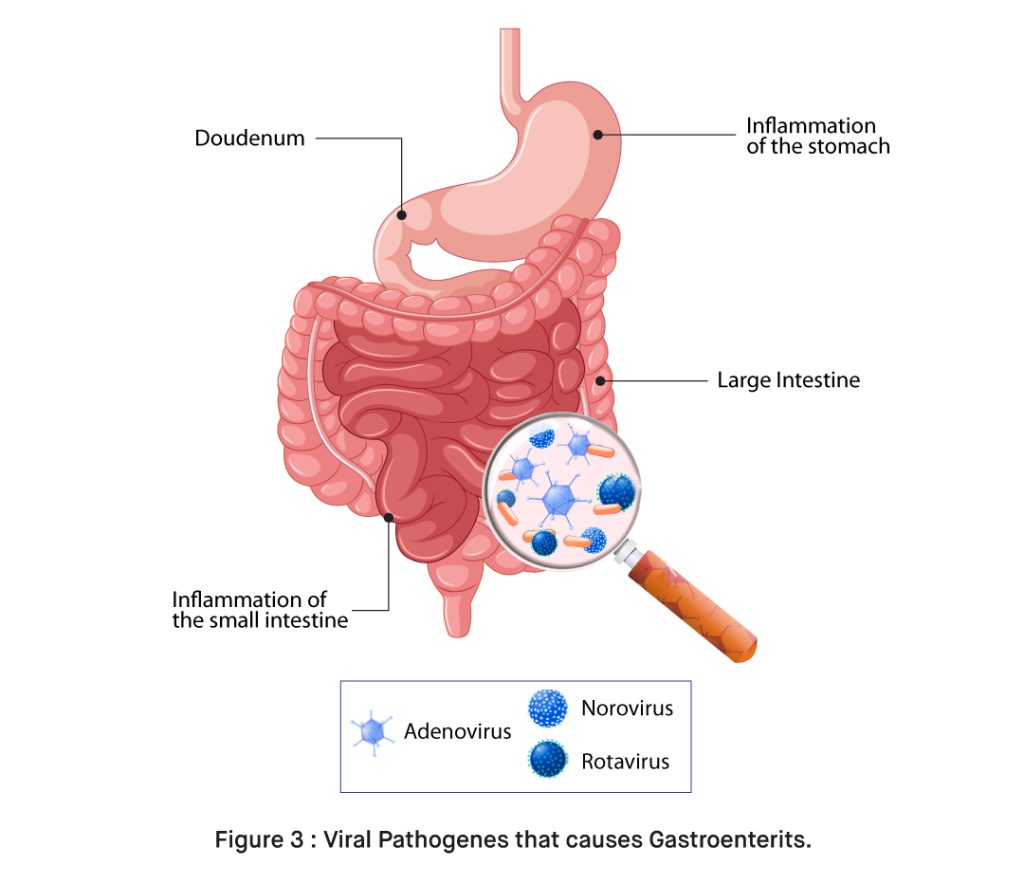
Viral Causes
- Norovirus – Common cause of adult gastroenteritis
- Rotavirus – Common in children <3 years; frequent outbreaks in day-care centres
- Transmission: Faecal-oral
- Incubation: ~2 days
- Duration: ~6 days
- Infective period: Up to 2 days after symptoms resolve
Morphology / Pathophysiology
- Viral pathogens (esp. rotavirus) damage enterocytes and secrete NSP4 protein → chloride secretion ↑ and water absorption ↓
- Bacterial toxins (e.g. from EHEC) may directly damage intestinal mucosa or systemically affect other organs (e.g. HUS)
Clinical Features
- General symptoms:
- Nausea, vomiting
- Abdominal cramps
- Watery or bloody diarrhoea
- Fever, myalgia, poor feeding in children
- Toxigenic diarrhoea: Onset within 4 hours, prominent vomiting
- Dysentery: Bloody diarrhoea (EIEC, EHEC, Salmonella)
- Cholera: Profuse watery diarrhoea without abdominal pain
Investigations
- History & clinical course – key to diagnosing foodborne outbreaks
- Stool tests (if required):
- Stool OCP (ova, cysts, parasites)
- Enzyme immunoassay
- RT-PCR
- Epidemiology – group outbreaks may suggest source
Management
- Supportive care is the mainstay of treatment
- Oral or IV fluid replacement (especially in children and elderly)
- Use the “421 Rule” for IV fluids:
- 4 ml/kg/hr (first 10kg)
- 2 ml/kg/hr (second 10kg)
- 1 ml/kg/hr (thereafter)
- Antibiotics:
- Reserved for specific cases (e.g. Typhoid → ceftriaxone, ciprofloxacin)
- Anti-diarrhoeals: Controversial (may impair toxin clearance)
- Quarantine: Prevent spread in healthcare/childcare settings
Complications
- Dehydration and electrolyte imbalance
- Haemolytic-Uraemic Syndrome (EHEC)
- Septicaemia (e.g. in typhoid)
- Bowel perforation (severe Salmonella infection)
Differential Diagnosis
- Appendicitis
- Inflammatory bowel disease (IBD)
- Irritable bowel syndrome (IBS)
- Medication-induced diarrhoea
- Parasitic infections (e.g. Giardia)
Summary – Gastroenteritis
Gastroenteritis is a high-yield clinical condition frequently encountered in both community and hospital settings. While most cases are self-limiting and viral, bacterial causes like EHEC, Salmonella, and Shigella may lead to serious complications. Final-year medical students must be able to distinguish between toxigenic, dysenteric, and viral causes, and manage with supportive care as first-line. For more, visit our Gastrointestinal Overview page.