Table of Contents
Overview – Acute Abdomen
Acute abdomen refers to the sudden onset of severe abdominal pain that may require urgent surgical intervention. Recognising critical patterns such as peritonitis, rupture, or colicky pain is essential in emergency medicine to triage patients appropriately. Prompt evaluation, resuscitation, and surgical consultation—when needed—can be lifesaving.
Definition
The term “acute abdomen” describes a clinical scenario of acute abdominal pain that often indicates a serious intra-abdominal pathology, sometimes requiring emergency surgery (e.g. laparotomy).
Aetiology
Conditions That May Require Laparotomy
- Organ Rupture:
- Spleen
- Aorta
- Ectopic pregnancy
→ Rapid blood loss → shock
- Peritonitis from Perforation:
- Peptic/Duodenal ulcer
- Diverticulum
- Appendicitis
- Bowel or gallbladder perforation
→ Prostration, shock, abdominal rigidity, absent bowel sounds
Conditions That Usually Do NOT Require Laparotomy
- Localised Peritonitis:
- Diverticulitis
- Cholecystitis
- Salpingitis
- Appendicitis
→ Stillness, guarding, localised rebound tenderness
- Colic (e.g. renal, biliary):
→ Restlessness, pain that waxes and wanes
Types of Abdominal Pain
1. Visceral Pain
- Originates from abdominal viscera
- Poorly localised, often periumbilical
- Fluctuating in intensity (colicky)
- Autonomic symptoms: nausea, sweating
- Patient tends to move frequently to get comfortable
2. Somatic/Parietal Pain
- Sharp, well-localised pain from peritoneal irritation
- Worsens with movement, coughing, or deep breathing
- Patient tends to stay very still
- Suggests involvement of the parietal peritoneum
3. Referred Pain
- Felt at a location distant from the source due to shared embryological origins
- Examples:
- Diaphragm → Shoulder tip
- Inferior MI → Epigastric pain
- Testicular torsion → Hypogastric pain
Clinical Assessment
History
- Pain behaviour:
- Constant vs. intermittent
- Worse with movement → suggests somatic origin
- Waxing/waning → colicky (e.g. obstruction)
- Progression:
- Visceral → Somatic (e.g. appendicitis)
- Associated symptoms:
- Vomiting, altered bowel habits, fever, haemodynamic instability
Examination
- Inspection and Palpation:
- Guarding, rebound, rigidity
- Auscultation:
- Absent bowel sounds in peritonitis
- Vital signs:
- Tachycardia, hypotension, altered consciousness
Investigations
- Bloods:
- U&E
- FBC
- LFTs
- CRP
- Amylase (pancreatitis?)
- ABG
- Urinalysis – rule out renal pathology
- Imaging:
- Erect CXR: Look for air under diaphragm (suggests perforation)
- Abdominal CT/US: As clinically indicated
Management
Immediate Priorities
- Resuscitation first!
- IV fluids
- Monitor vitals
- Correct shock before anaesthesia (anaesthesia worsens hypotension)
Surgical Consultation
- Indicated for suspected perforation, rupture, or peritonitis
- Laparotomy may be necessary
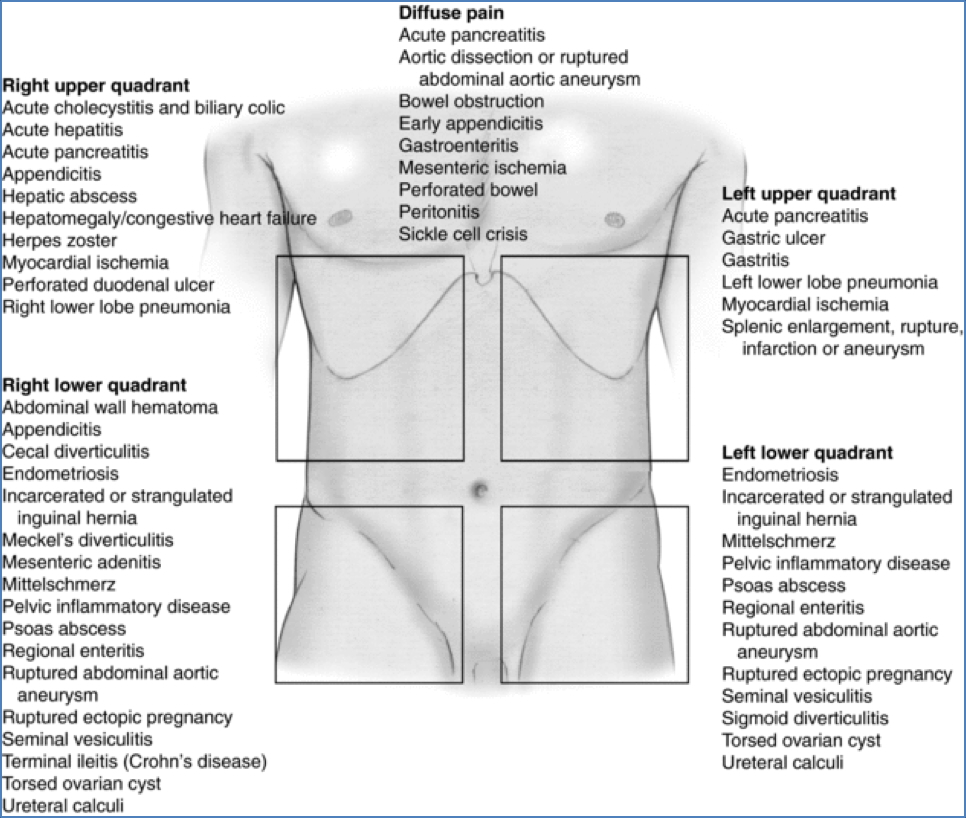
Differential Diagnosis
- Appendicitis
- Diverticulitis
- Peptic ulcer perforation
- Ectopic pregnancy
- Bowel obstruction
- Renal or biliary colic
- Myocardial infarction
- Testicular torsion
- Gastroenteritis
- Inflammatory bowel disease
Summary – Acute Abdomen
Acute abdomen is a time-critical clinical presentation that encompasses a wide range of underlying causes, some of which are life-threatening and require surgical intervention. Accurate assessment of pain type (visceral vs. parietal), associated features, and prompt resuscitation can guide effective triage and management. For a broader context, see our Gastrointestinal Overview page.