Table of Contents
Overview – Psoriatic Arthritis
Psoriatic arthritis is a chronic, immune-mediated inflammatory arthritis that occurs in association with psoriasis. It often presents with symmetrical distal joint involvement, dactylitis, and enthesitis, alongside classic psoriatic skin changes such as plaque psoriasis and onycholysis. Recognising psoriatic arthritis early is essential to reduce joint damage, improve quality of life, and coordinate care with dermatology and rheumatology teams.
Definition
Psoriatic arthritis is a seronegative spondyloarthropathy that develops in patients with psoriasis, involving both joint and skin pathology. It typically affects the distal interphalangeal (DIP) joints, but may present in several different patterns.
Aetiology
- Complication of psoriasis (seen in up to 30% of cases)
- Genetic and immunologic association
- Strong familial clustering
- HLA-B27 may be present in axial involvement
- Often manifests in young to middle-aged adults
Pathogenesis
- Autoimmune T-cell infiltration of skin and joint synovium
- Leads to chronic inflammation, synovitis, and joint damage
- Involves both innate and adaptive immunity
Clinical Features
Cutaneous Features
- Psoriasis vulgaris
- Red plaques with silvery scales (due to hyperkeratosis and parakeratosis)
- Nail changes
- Onycholysis (nail separation from nail bed)
- Nail pitting
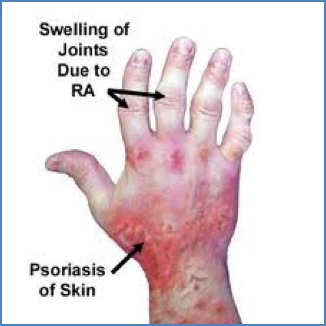
Articular Features
- Symmetrical arthritis of DIP joints (can resemble RA but seronegative)
- Dactylitis (“sausage digits”)
- Enthesitis
- Commonly Achilles tendonitis and plantar fasciitis
- Axial involvement may occur (less common than in ankylosing spondylitis)


Ocular Features
- Conjunctivitis
- Anterior uveitis/iritis
Investigations
- Primarily clinical diagnosis
- Rheumatoid factor and anti-CCP antibodies usually negative
- Imaging:
- Joint X-rays may show pencil-in-cup deformities in DIP joints
- Enthesitis and joint space narrowing in chronic disease
Management
- DMARDs
- Methotrexate
- Sulfasalazine
- Corticosteroids – for acute flares
- Biologics (e.g. TNF inhibitors) if refractory
- Skin management
- Moisturizers
- Topical steroids
- Phototherapy
Complications
- Progressive joint damage and deformity
- Reduced functional capacity
- Associated with metabolic syndrome and cardiovascular risk
- Psychological comorbidity due to chronic skin/joint disease
Differential Diagnosis
- Rheumatoid arthritis
- Osteoarthritis
- Reactive arthritis
- Gout
- Ankylosing spondylitis
Summary – Psoriatic Arthritis
Psoriatic arthritis is a chronic autoimmune arthritis associated with psoriasis, affecting both the joints and skin. It commonly presents with DIP joint arthritis, dactylitis, and nail changes, and is managed using DMARDs, corticosteroids, and targeted skin therapies. For a broader context, see our Musculoskeletal Overview page.