Table of Contents
Overview – Mood Stabilising Drugs
Mood stabilising drugs are a cornerstone in the pharmacological treatment of affective disorders, particularly bipolar disorder and recurrent depression. These agents target dysregulation in neurotransmitter signalling — primarily norepinephrine (NA), serotonin (5HT), and dopamine — by modulating their reuptake, breakdown, and receptor activity. This article outlines the key classes, mechanisms, and adverse profiles of mood stabilising drugs relevant to final-year medical exams and clinical practice.
Definition
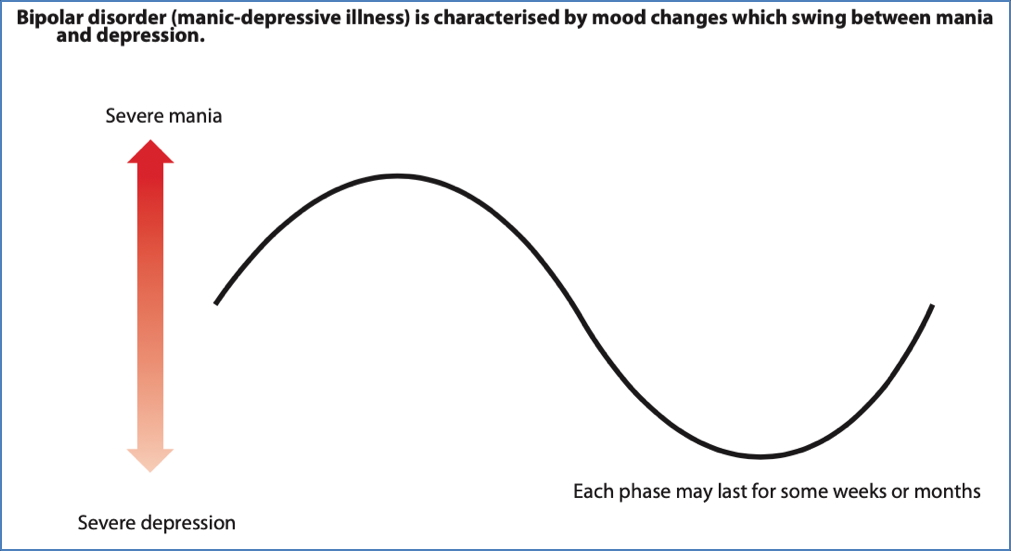
Mood stabilising drugs are pharmacological agents that reduce the frequency, intensity, and duration of mood fluctuations in patients with affective disorders, particularly bipolar affective disorder and treatment-resistant depression. These include antidepressants and agents with anti-manic properties, such as lithium and certain anticonvulsants.
Mechanism of Action
The dominant hypothesis for mood disorders is the Monoamine Hypothesis:
- Depression = deficiency in norepinephrine and/or serotonin
- Mania = excess of the same neurotransmitters
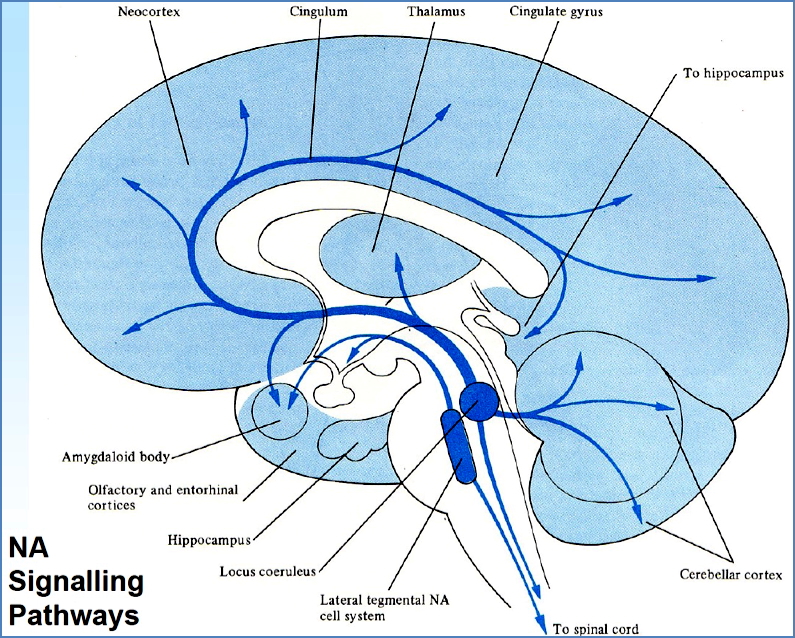
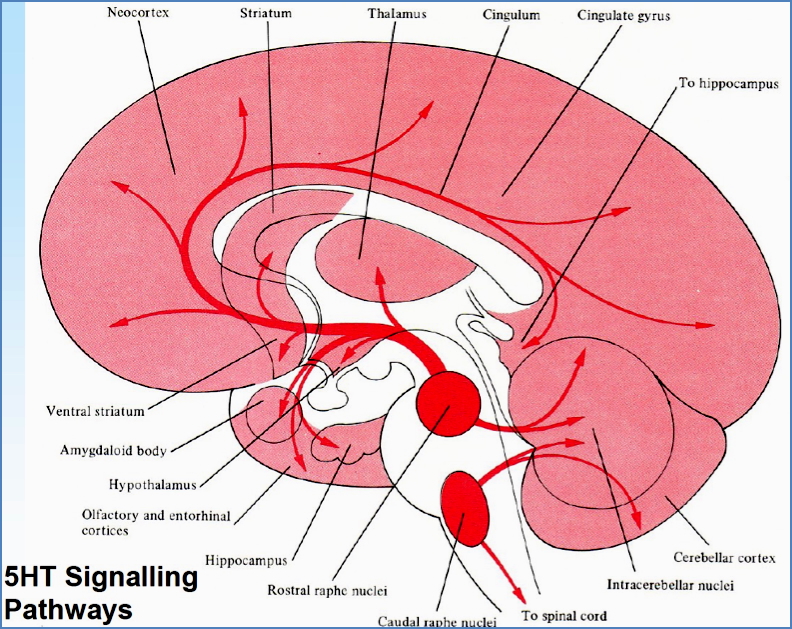
(Note: 5HT is the Neurotransmitter of Sleep, Mood, Feeding & Appetite)
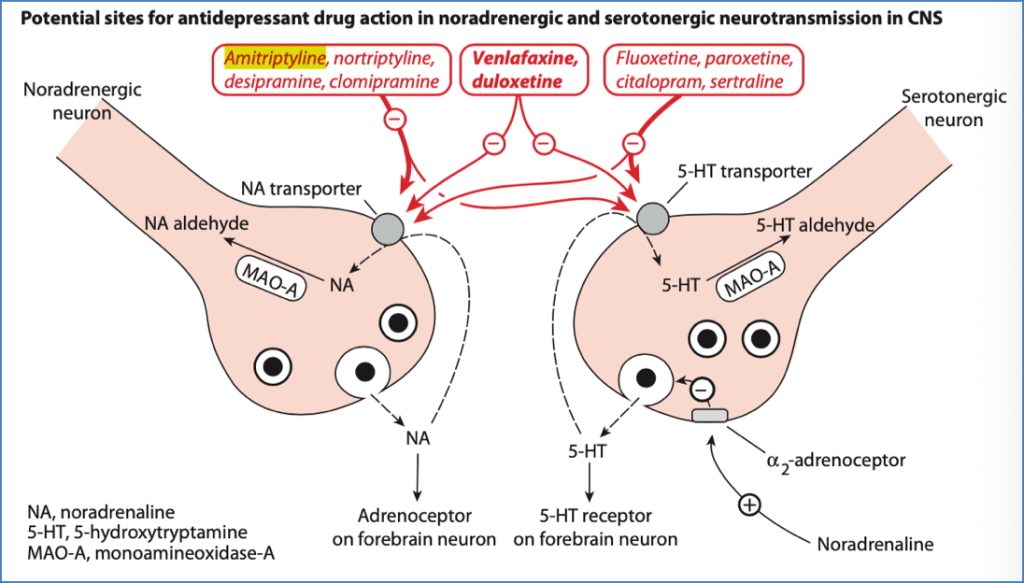
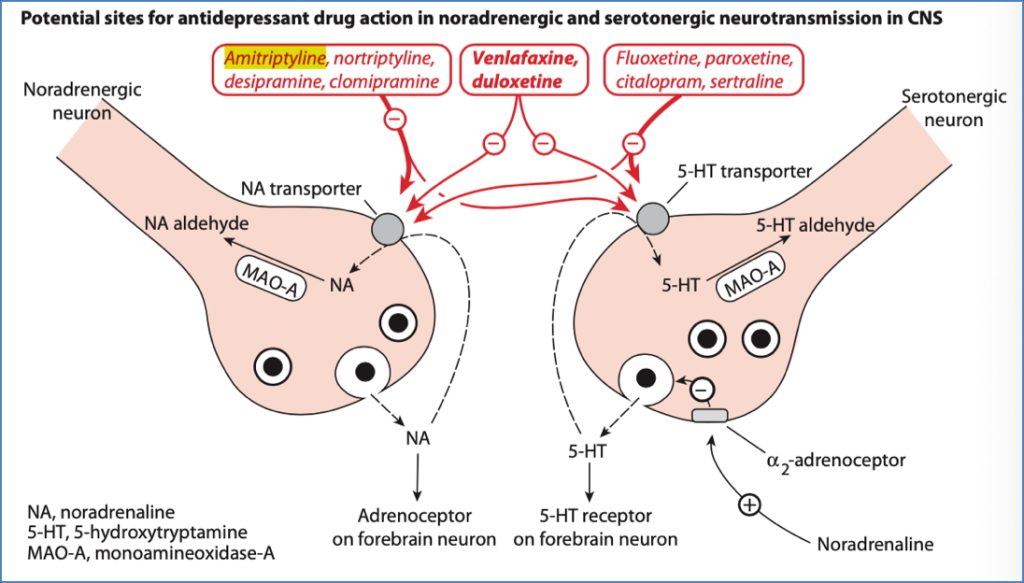
Drug targets include:
- Reuptake inhibition of NA/5HT → prolongs synaptic availability
- MAO inhibition → prevents breakdown of monoamines
- Presynaptic autoreceptor blockade → enhances NT release
- Post-synaptic receptor sensitivity modulation
Drug Classes
1. Tricyclic & Tetracyclic Antidepressants (TCAs)
- Mechanism: Inhibit reuptake of both NA and 5HT
- Examples: Imipramine, Amitriptyline
- Adverse Effects:
- Sedation
- Anticholinergic: dry mouth, constipation, urinary retention
- Postural hypotension
- Overdose risk: convulsions, arrhythmias, coma
2. Selective Serotonin Reuptake Inhibitors (SSRIs)
- Mechanism: Selectively block serotonin reuptake
- Example: Fluoxetine (Prozac)
- Adverse Effects:
- GI upset (nausea, diarrhoea)
- Anorexia
- Insomnia
- Sexual dysfunction (↓libido, anorgasmia)
3. Selective Noradrenaline Reuptake Inhibitors (SNRIs)
- Mechanism: Inhibit NA reuptake; α2 antagonist effects
- Example: Mianserin
- Adverse Effects: Similar to TCAs
- Sedation, antimuscarinic symptoms
- Overdose: convulsions, coma, arrhythmias
4. Monoamine Oxidase Inhibitors (MAOIs)
- Mechanism: Inhibit MAO → prevents NT breakdown → ↑NA/5HT
- Example: Phenelzine
- Adverse Effects:
- Hypotension
- Tremor, insomnia
- Weight gain
- Antimuscarinic effects
- Tyramine interaction:
- Tyramine is normally metabolised by MAO
- Inhibition leads to accumulation → NA release → hypertensive crisis
- Symptoms: ↑BP, tachycardia, risk of stroke/MI
5. Lithium Carbonate
- Indication: Bipolar disorder (anti-manic + antidepressant)
- Mechanism:
- ↑ Serotonin transmission
- ↓ Noradrenaline activity
- Alters Na⁺ transport
- Inhibits inositol phosphate signalling
- Adverse Effects:
- Tremor
- GI upset
- Renal impairment
- Thyroid dysfunction
- Narrow therapeutic index → monitor plasma levels
6. Anticonvulsants as Mood Stabilisers
- Mechanism: Enhance GABAergic tone → reduces neuronal excitability
- Common agents: Sodium valproate, carbamazepine, lamotrigine
- Advantages: Less toxic than lithium; fewer endocrine/renal effects
- Use: First-line for patients intolerant to lithium or with rapid-cycling bipolar disorder
Serotonin Syndrome
Trigger: Combination or overdose of serotonergic drugs (e.g., SSRIs, TCAs, MAOIs)
Clinical features:
| Domain | Symptoms |
|---|---|
| Cognitive | Agitation, delirium, confusion, coma |
| Autonomic | Hyperthermia, tachycardia, BP lability, sweating, dilated pupils |
| Gastrointestinal | Nausea, vomiting, diarrhoea |
| Neuromuscular | Tremor, clonus, hyperreflexia, myoclonus, ataxia |
| Haematological | ↑ CK, leukocytosis, DIC, thrombocytopenia |
Complimentary Agents
St John’s Wort
- Mechanism:
- ↓ Beta-adrenergic receptors
- ↑ 5HT₂ receptors in cortex
- Clinical Use: Mild to moderate depression
- Risks:
- Significant drug interactions with SSRIs, warfarin, OCPs, etc.
- May precipitate serotonin syndrome in combination therapy

Summary – Mood Stabilising Drugs
Mood stabilising drugs act via a range of pharmacological mechanisms targeting serotonin, norepinephrine, and GABA pathways to treat depression and bipolar disorder. Classes include antidepressants (SSRIs, TCAs, MAOIs), lithium, and anticonvulsants. These drugs must be chosen and monitored carefully due to varying side effect profiles, toxicities, and interactions. For a broader context, see our Pharmacology & Toxicology Overview page.