Table of Contents
Overview – Male Reproductive Anatomy
Male reproductive anatomy encompasses the organs responsible for sperm production, maturation, and delivery. These include the testes, epididymis, vas deferens, penis, prostate, and accessory glands. Understanding this anatomy is essential for grasping clinical concepts such as male infertility, testicular torsion, prostate pathology, and sexually transmitted infections.
Definition
The male reproductive system consists of internal and external structures responsible for producing, storing, and delivering sperm, as well as synthesising and secreting sex hormones—primarily testosterone.
Ducts of the Male Reproductive Tract
These structures transport sperm and form part of the ejaculatory pathway.
- Epididymis
- Coiled tubules on the posterior testis
- Site of sperm maturation
- Contributes ~5% of ejaculate volume
- Ductus (Vas) Deferens
- Thick-walled duct transporting sperm from epididymis to ejaculatory ducts
- Lined with pseudostratified columnar epithelium with surrounding smooth muscle
- Urethra
- Terminal passage for semen and urine
- Divided into:
- Prostatic urethra
- Membranous urethra
- Spongy (penile) urethra
- External urethral orifice
- Lined by transitional epithelium (in proximal segments)
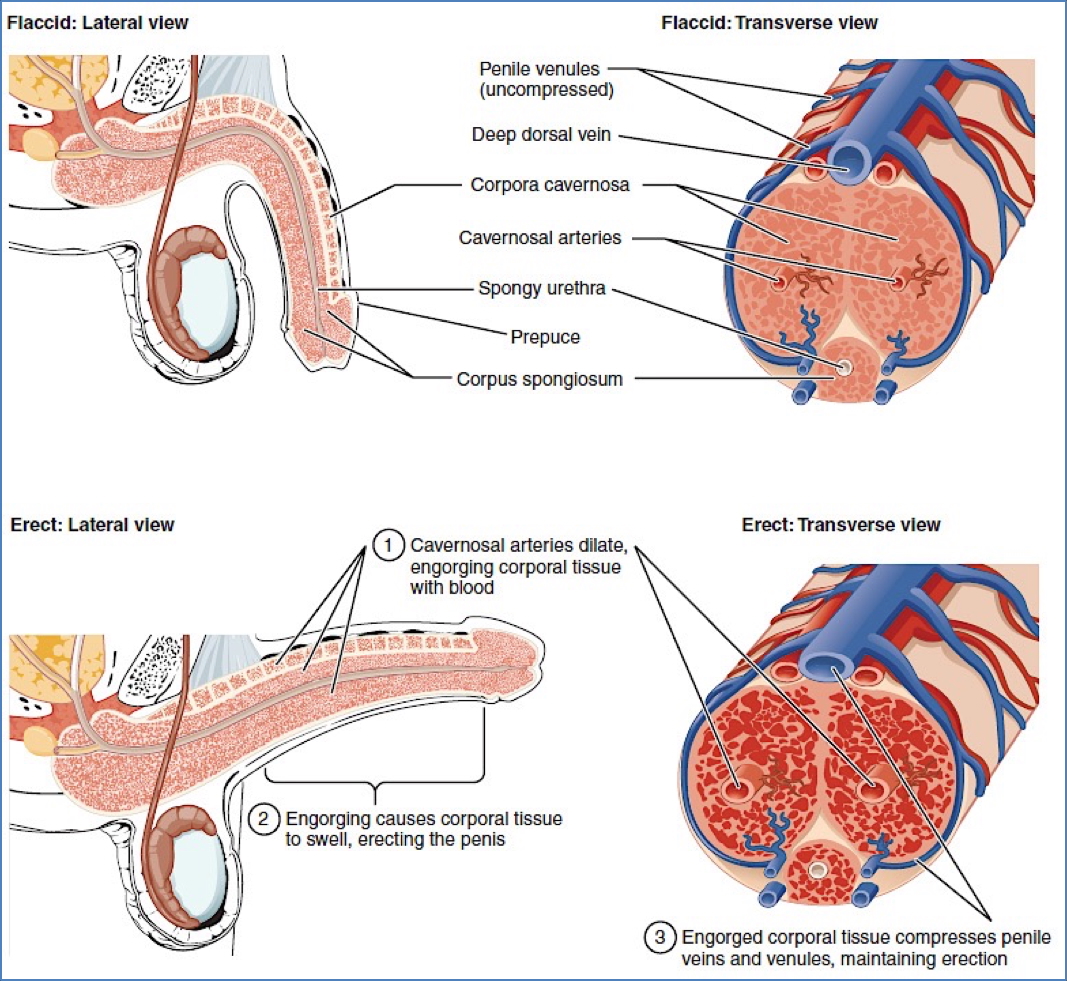
Penis
- Composed of three regions:
- Root
- Body (shaft)
- Glans penis
- Erectile tissues
- 2x Corpus Cavernosum – contain central arteries for erection
- 1x Corpus Spongiosum – surrounds urethra and prevents compression during erection
- Other features
- Corona: ridge at base of glans
- Prepuce: foreskin (may be retracted or removed)
- Tunica Albuginea: dense fibrous sheath enclosing corpora cavernosa and testis, not the epididymis

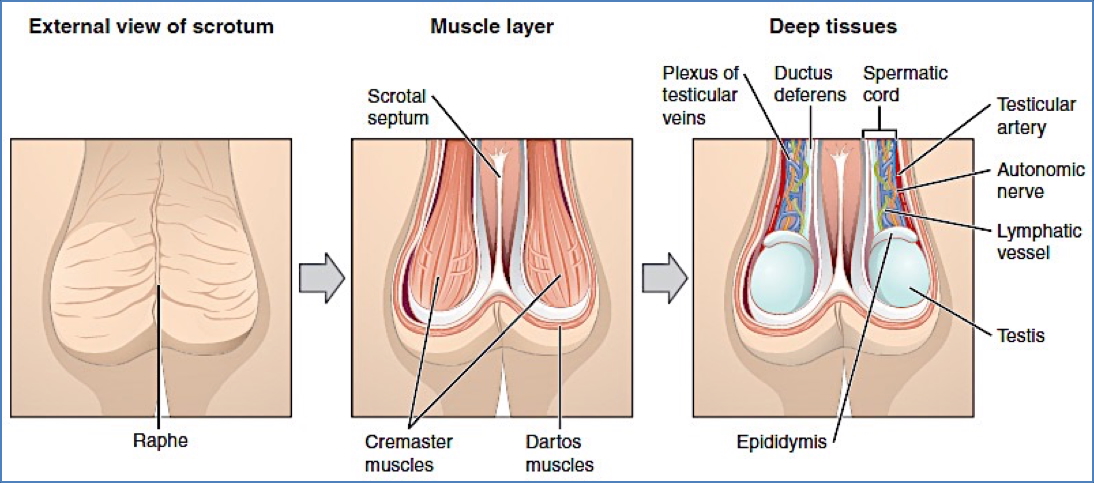
Testicles & Scrotum
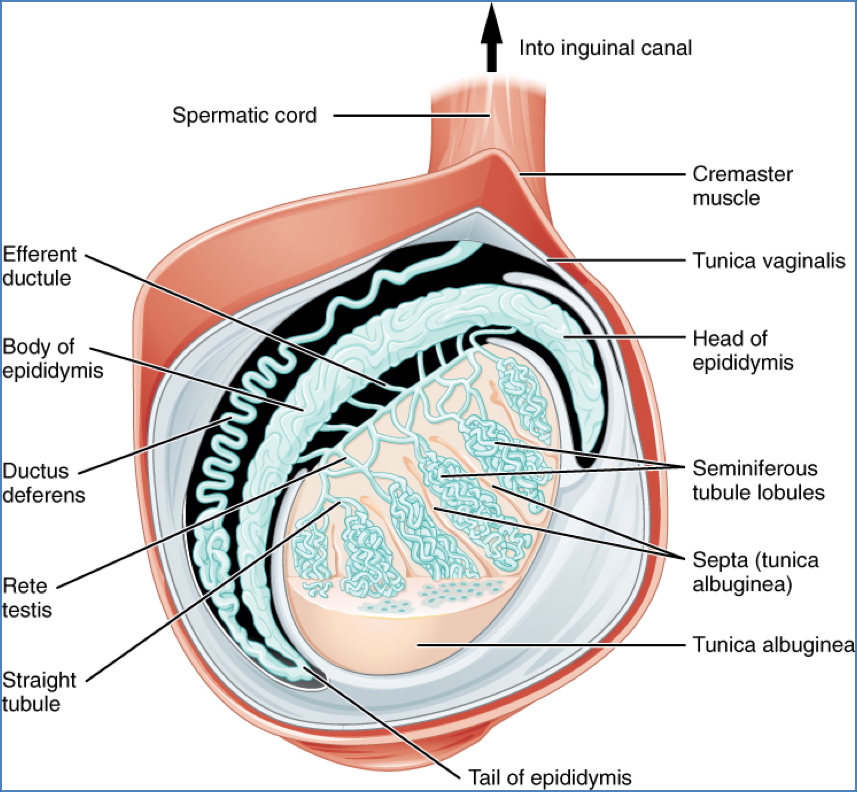
- Testes
- Male gonads that produce sperm and testosterone
- Enclosed by Tunica Albuginea
- Contain:
- Seminiferous tubules: site of spermatogenesis
- Leydig cells: located interstitially; secrete testosterone in response to luteinising hormone (LH)
- Epididymis
- Lined by pseudostratified columnar epithelium
- Maturation and storage of sperm
- Spermatic Cord
- Contains:
- Vas deferens
- Testicular artery
- Pampiniform venous plexus
- Lymphatics
- Contains:
- Tunica Vaginalis
- Peritoneal remnant dragged into the scrotum during testicular descent
- Failure to obliterate processus vaginalis may → indirect inguinal hernia
- Thermoregulation
- Testes remain outside the body due to optimal temperature for spermatogenesis
- Cremaster muscle: elevates testis in response to cold
- Dartos muscle: adjusts scrotal surface area
- Pampiniform plexus
- Network of veins aiding in heat exchange to maintain testicular temperature
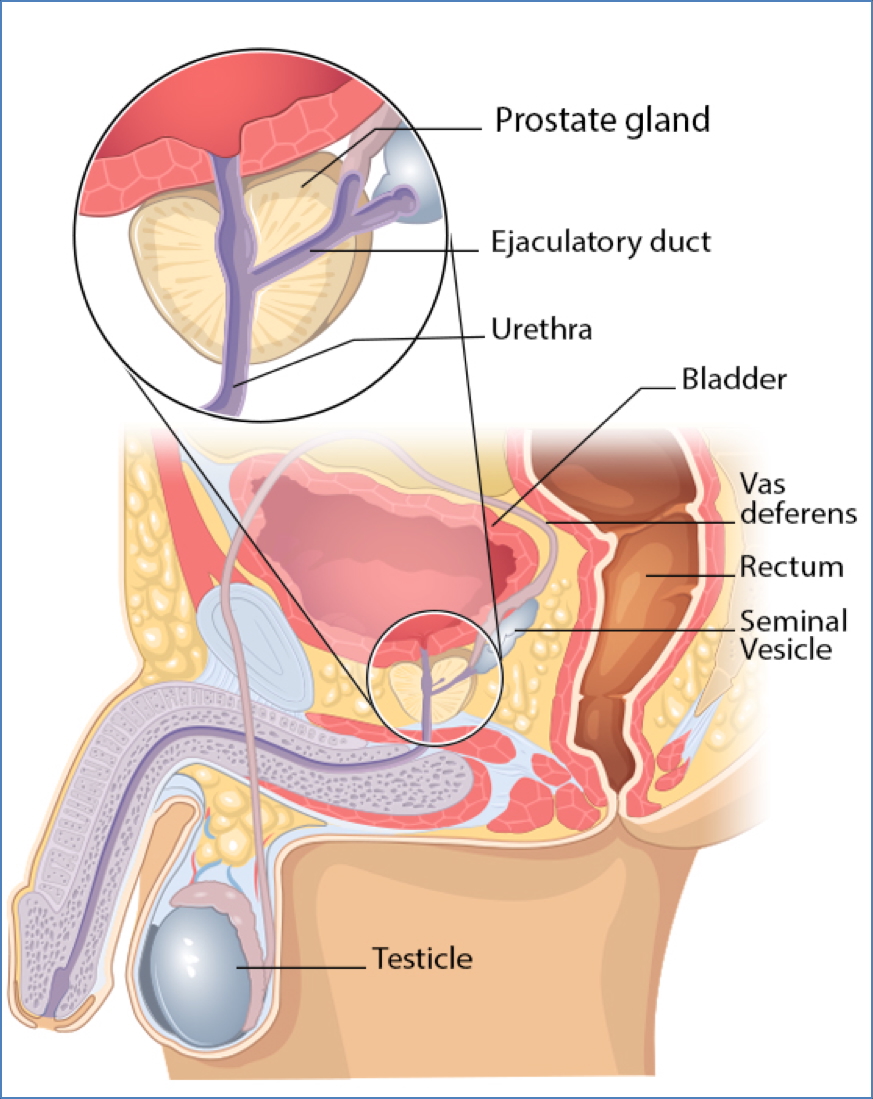
Accessory Glands
These glands contribute to seminal fluid:
- Seminal Vesicles
- ~60% of ejaculate
- Fructose-rich, alkaline secretion that reduces semen acidity
- Prostate Gland
- ~30% of ejaculate
- Produces fluid that activates and nourishes sperm
- Bulbourethral (Cowper’s) Glands
- ~5% of ejaculate
- Secrete alkaline mucus to neutralise urinary acidity in urethra
The Prostate Gland
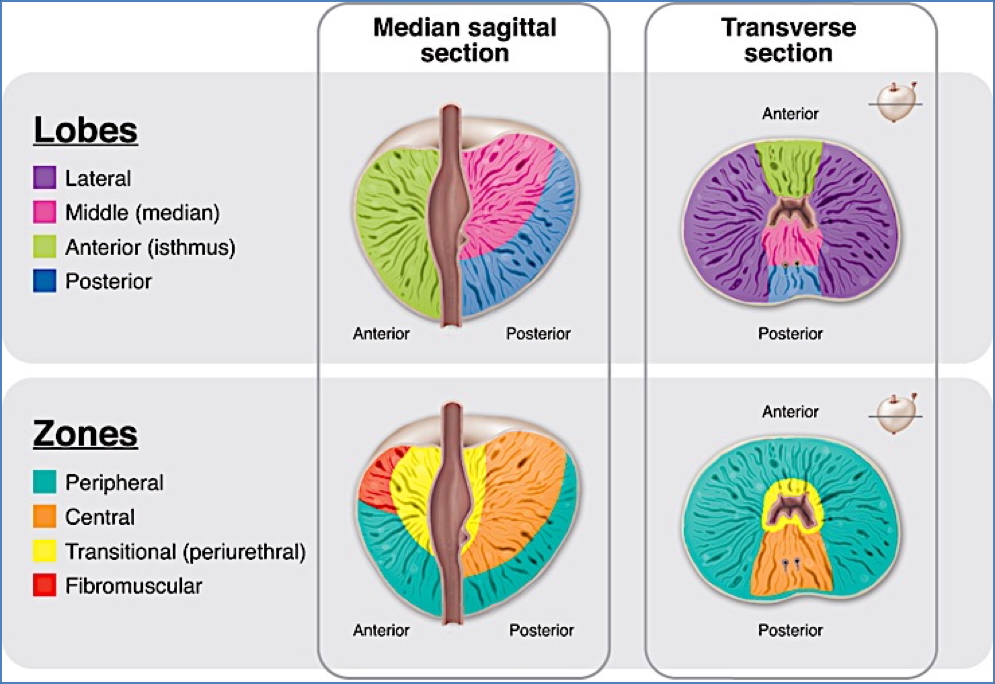
Anatomy
- Situated inferior to bladder, posterior to pubic symphysis
- Surrounds the urethra (periurethral location)
- Encases ejaculatory ducts from seminal vesicles
- Divided into 5 lobes:
- Anterior
- Posterior
- Median
- Left & Right lateral lobes
Function
- Secretes proteolytic enzymes contributing to semen liquidity
- Acid phosphatase & Prostate-Specific Antigen (PSA) maintain fluid state
- Responsive to androgen stimulation
Histology
- Fibromuscular organ with abundant smooth muscle
- Normal prostatic glands have double-layered epithelium
- Note: Prostate cancer typically shows single-layer epithelium
2. https://shri.public-health.uiowa.edu/wp-content/uploads/2019/10/Prostate-1-Intro_Anatomy.pdf
Structures Involved in Spermatogenesis
- Seminiferous Tubules
- Contain:
- Sertoli Cells
- Line the tubule walls
- Create the blood-testis barrier
- Respond to follicle-stimulating hormone (FSH) → secrete androgen-binding protein (keeps testosterone levels high for spermatogenesis)
- Germ Cells (Spermatogonia)
- At varying stages of development
- Luminal spermatids have visible tails
- Sertoli Cells
- Contain:
- Leydig Cells
- Found in the interstitial space outside tubules
- Produce testosterone in response to LH
- Epididymis & Vas Deferens
- Sites of sperm maturation and transport
- Both lined with pseudostratified columnar epithelium

Summary – Male Reproductive Anatomy
The male reproductive anatomy comprises structures that produce, store, and deliver sperm, along with glands that contribute to seminal fluid. Key organs include the testes, epididymis, vas deferens, penis, prostate, and seminal vesicles. Each plays a critical role in reproduction, hormonal regulation, and clinical conditions such as infertility or prostate disease. For a broader context, see our Reproductive Health Overview page.