Table of Contents
Overview – Polycystic Ovarian Syndrome
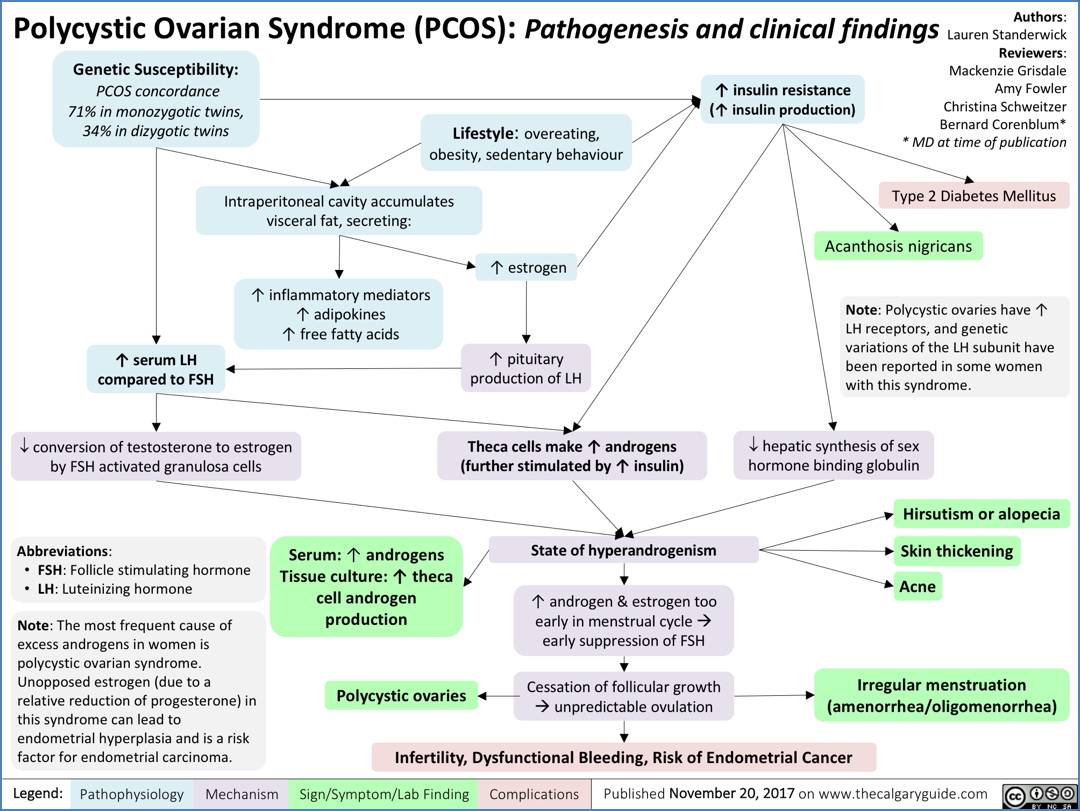
Polycystic ovarian syndrome (PCOS) is a common endocrine disorder in women of reproductive age, characterised by hyperandrogenism, menstrual irregularity, and polycystic ovaries. It arises from disrupted hypothalamo-pituitary-ovarian signalling and is associated with infertility, metabolic syndrome, and increased long-term risks including endometrial cancer and type 2 diabetes. Timely recognition and multidisciplinary management are key.
Definition
Polycystic ovarian syndrome (PCOS) is a hormonal disorder defined by at least two of the following (Rotterdam criteria):
- Oligo- or anovulation
- Clinical and/or biochemical signs of hyperandrogenism
- Polycystic ovaries on ultrasound
Aetiology
- Genetic: Sex-limited autosomal dominant inheritance
- ~50% chance of inheritance if female offspring
- Environmental/metabolic factors influence expression (e.g. obesity, insulin resistance)
Pathogenesis
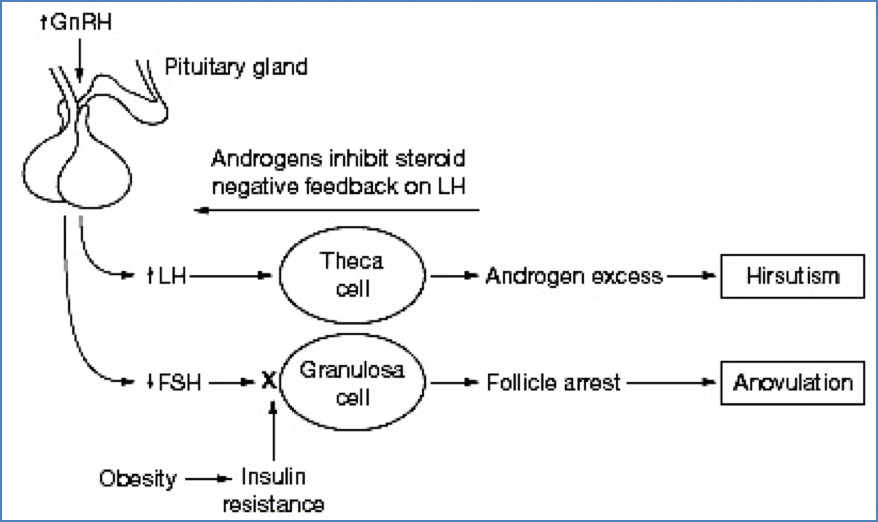
- Disruption of the hypothalamo-pituitary-gonadal axis:
- ↑ Gonadotropin-releasing hormone (GnRH) pulsatility
- ↑ Luteinising hormone (LH) and ↓ Follicle-stimulating hormone (FSH)
→ Stimulates thecal cells to produce excess androgens
→ Suppressed granulosa cell function → follicular arrest
- Follicular arrest:
- Follicles grow to mid-antral stage but fail to mature
- Granulosa layer thins over time → poor oestrogen conversion
- Result: Persistent anovulation + hyperandrogenism
Morphology
- Polycystic ovaries on ultrasound:
- Enlarged ovaries with >12 peripheral immature follicles
- Described as a “string of pearls” appearance

Clinical Features
Reproductive Features
- Oligomenorrhoea or amenorrhoea
- Anovulation → infertility, recurrent miscarriage
- Enlarged, cystic ovaries
Hyperandrogenism
- Acne
- Hirsutism (excess body/facial hair)
- Deepening of voice
- Elevated serum testosterone
Metabolic Dysfunction
- Insulin resistance
- Obesity
- Dyslipidaemia
- Increased risk of type 2 diabetes mellitus (D2M)
- Increased risk of hypertension and cardiovascular disease
Long-Term Risks
- Unopposed oestrogen exposure → endometrial hyperplasia/cancer
- Fertility challenges
- Metabolic syndrome (Syndrome X)
Diagnosis
- Clinical features: Menstrual irregularity, hirsutism, acne
- Pelvic ultrasound: Bilateral polycystic ovaries
- Blood tests:
- ↑ Serum testosterone
- Rule out differentials:
Management
Treatment Goals
- Reverse signs of androgen excess
- Restore ovulation and menstrual regularity
- Improve fertility
- Prevent metabolic complications
First-Line Treatments
- Combined oral contraceptive pill (COCP) or IUD
- Regulates menstruation, reduces hirsutism
- Anti-androgens (e.g. spironolactone)
- Weight loss and lifestyle changes
- Improves insulin sensitivity
- Reduces risk of diabetes and cardiovascular disease
- Metformin
- Improves insulin resistance
- Promotes ovulation and fertility
Fertility-Focused Treatment
- Ovulation induction: Clomiphene citrate, letrozole, or gonadotropins
- Consider referral to fertility specialist if unsuccessful
Prognosis
Women with PCOS have increased lifelong risks of:
- Endometrial cancer (due to unopposed oestrogen)
- Type 2 diabetes mellitus
- Hypertension and cardiovascular disease
- Persistent subfertility if not adequately managed
Summary – Polycystic Ovarian Syndrome
Polycystic ovarian syndrome (PCOS) is a genetic and hormonal condition marked by hyperandrogenism, irregular menstruation, and metabolic dysfunction. It presents a major cause of infertility and carries increased risks of type 2 diabetes and endometrial cancer. Management targets symptom relief, menstrual regulation, fertility, and metabolic risk reduction. For a broader context, see our Reproductive Health Overview page.