Table of Contents
Overview – Endometrial Hyperplasia
Endometrial hyperplasia is a condition characterised by abnormal thickening of the endometrial lining, usually due to unopposed oestrogen stimulation. This can lead to heavy and prolonged menstrual bleeding, and in some cases, may progress to endometrial carcinoma—especially in atypical subtypes. A common cause of menorrhagia in women of reproductive age and perimenopausal women, understanding its pathophysiology and management is crucial for final-year medical students.
Definition
Endometrial hyperplasia refers to the abnormal proliferation of the endometrial glands resulting in thickened endometrial tissue. It occurs without invasion into the myometrium (which differentiates it from adenomyosis).
Aetiology
- Hyperestrogenaemia:
- Obesity
- Polycystic ovarian syndrome (PCOS)
- Unopposed oestrogen hormone replacement therapy (HRT)
- Tamoxifen use (ironically acts as an oestrogen agonist in the uterus despite being an oestrogen receptor blocker)
Pathophysiology
- Elevated oestrogen levels → Stimulate endometrial glandular proliferation
- Absence of progesterone’s counter-regulatory effect → Uncontrolled endometrial thickening
- This leads to:
- Menorrhagia (heavy/prolonged bleeding lasting 8–14 days)
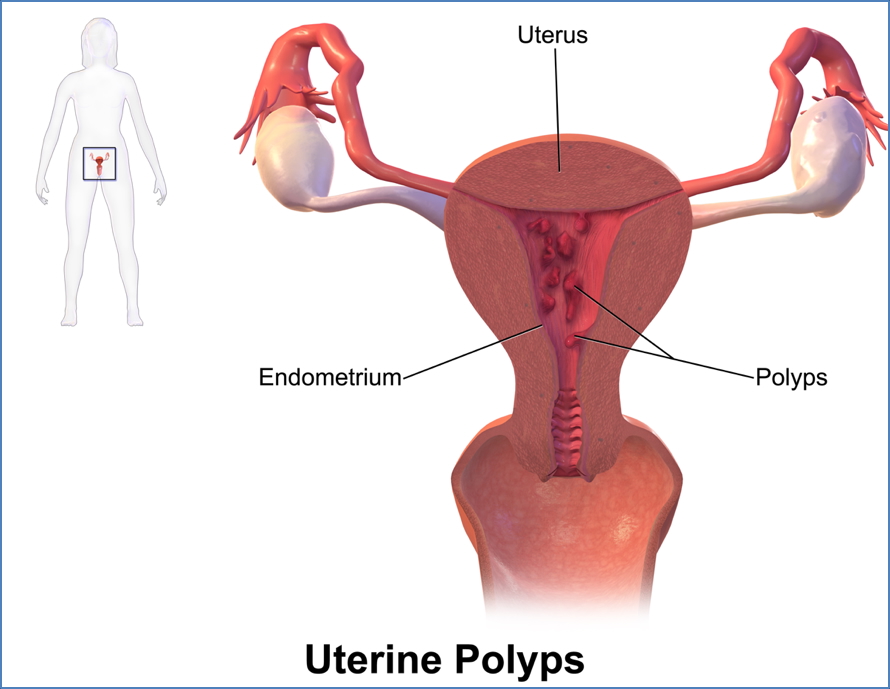
- In some cases, development of endometrial polyps
- Risk of progression to endometrial carcinoma, particularly in the atypical form
Morphology
Macroscopic
- Presence of single or multiple polyps in the uterine cavity
- Diffuse thickening of the endometrial lining
Microscopic (Histological Subtypes)
- Simple hyperplasia: Dilated, irregular, cystic glands
- Complex hyperplasia: Glandular crowding and budding
- Atypical hyperplasia: Cellular atypia (nuclear enlargement, stratification, pleomorphism, increased mitoses)
Clinical Features
- Menorrhagia: Heavy or prolonged menstrual bleeding (lasting 8–14 days)
- May be asymptomatic in early stages
- Rarely: Intermenstrual bleeding or postmenopausal bleeding
Investigations
- Transvaginal ultrasound (TVUS):
- Endometrial thickness >5 mm (especially significant in postmenopausal women)
- Endometrial biopsy (via curettage or pipelle):
- Essential for histological classification
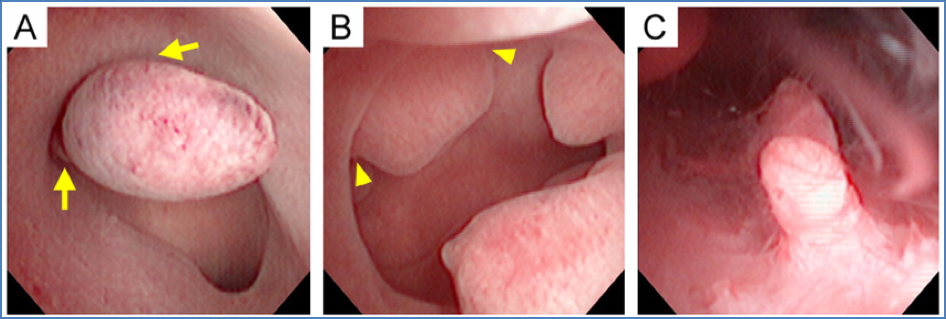
- Hysteroscopy:
- Direct visualisation and biopsy of suspected polyps
Management
Medical
- Progesterone-only contraceptives (e.g. oral, Mirena IUD, Implanon):
- Suppress endometrial proliferation
- Effective in managing menorrhagia and reducing progression risk
Surgical
- Hysterectomy:
- Considered in recurrent, atypical, or refractory cases
- Especially indicated in women at risk of malignancy or not wishing to preserve fertility
Complications
- Endometrial carcinoma, particularly in atypical hyperplasia
- Anaemia due to chronic heavy menstrual bleeding
Differential Diagnosis
- Adenomyosis
- Uterine fibroids
- Dysfunctional uterine bleeding
- Endometrial carcinoma
- Coagulopathies
Summary – Endometrial Hyperplasia
Endometrial hyperplasia is a hormone-driven condition where excess oestrogen leads to thickened endometrial tissue and heavy menstrual bleeding. It can present with or without polyps and ranges from benign to premalignant forms depending on histology. For a broader context, see our Reproductive Health Overview page.