Table of Contents
Overview – Vaginitis and Vaginosis
Vaginitis and vaginosis are common causes of vaginal discharge and discomfort in women, most often caused by bacterial, fungal, or protozoan infections. Bacterial vaginosis (BV), candidiasis (thrush), and trichomoniasis each have distinct presentations, diagnostic features, and treatments. Although usually benign, these conditions may significantly affect quality of life and can have implications for sexual health and pregnancy outcomes.
Definition
Vaginitis and vaginosis refer to inflammation or imbalance in the vaginal microbiota, typically due to infection.
- Vaginosis refers to bacterial imbalance without inflammation (e.g., bacterial vaginosis).
- Vaginitis implies infection with associated inflammation (e.g., candidiasis, trichomoniasis).
Aetiology
- Bacterial Vaginosis (50%): Gardnerella vaginalis
- Fungal Infection (30%): Candida albicans
- Protozoal Infection (20%): Trichomonas vaginalis
Pathogenesis
Bacterial Vaginosis – Gardnerella vaginalis
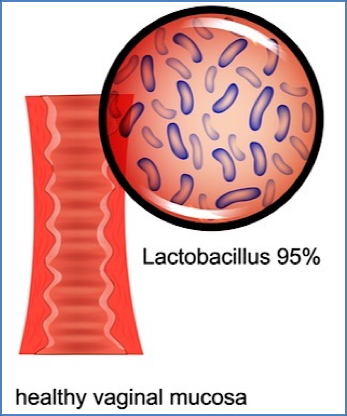
- Loss of normal Lactobacillus flora or vaginal acidity → overgrowth of anaerobic bacteria
Fungal Vaginitis – Candida albicans
- Overgrowth triggered by:
- Antibiotic use
- Immunosuppression (HIV, diabetes, corticosteroids)
- Excessive vaginal douching
- Common in immunocompromised hosts
Protozoal Vaginitis – Trichomonas vaginalis
- Transmitted sexually or via bowel flora contamination
- Infects the vagina and lower urinary tract
Morphology
Microscopy
- Normal Flora: Gram-positive lactobacilli
- Gardnerella: “Clue cells” (vaginal epithelial cells covered in bacteria)
- Candida: “Pseudohyphae” and budding yeast
- Trichomonas: Pear-shaped, flagellated protozoa

Clinical Features
All three infections may present with:
- Vaginal discharge
- Vulvovaginal irritation or pruritus
- Dyspareunia
Gardnerella (Bacterial Vaginosis)
- Thin, grey-white, homogeneous discharge
- Fishy odour (especially after intercourse)
- Mild vulval irritation
Candida (Fungal Vaginitis / “Thrush”)
- Thick, curd-like, white discharge
- Vulvovaginal erythema and pruritus
- Excoriation from scratching
- Dyspareunia and spotting

Trichomonas (Protozoal Vaginitis)
- Frothy, yellow-green discharge
- “Strawberry vagina” (punctate haemorrhages on cervix)
- Mild pruritus and dysuria
Investigations
- History: Discharge characteristics, recent antibiotics, sexual history, STI risk, diabetes
- Pelvic examination
- Vaginal pH testing:
- BV: pH >4.5
- Microscopy:
- “Clue cells” → BV
- “Pseudohyphae” → Candida
- “Motile flagellates” → Trichomonas
- PCR or NAAT for Trichomonas
- Discharge MCS (Microscopy, Culture & Sensitivity)
Management
Bacterial Vaginosis (Gardnerella)
- Metronidazole oral BD for 7 days
Candidiasis (Candida albicans)
- Fluconazole (oral), or topical clotrimazole or nystatin
- Address predisposing factors (e.g., stop douching, manage diabetes)
Trichomoniasis
- Metronidazole stat dose
- Treat sexual partners
- Avoid intercourse until resolution
Summary – Vaginitis and Vaginosis
Vaginitis and vaginosis, typically caused by Gardnerella vaginalis, Candida albicans, or Trichomonas vaginalis, are frequent causes of vaginal discharge and discomfort. Accurate diagnosis relies on history, microscopy, and pH testing, while management varies depending on the infective agent. For more on related gynaecological infections, see our Reproductive Health Overview page.