Table of Contents
Overview – Immune System Overview
The immune system overview provides a comprehensive foundation for understanding how the body recognises and defends against infections, cancer, and foreign materials. This complex yet coordinated functional system—comprising both the innate and adaptive immune systems—operates through molecular signals, immune cells, and antigen-presenting mechanisms. Mastery of this topic is crucial for final-year medical students to grasp the pathogenesis of infections, autoimmune conditions, immunodeficiencies, and the principles of immunotherapy.
Definition
- The immune system is a functional system, not confined to a single organ.
- Composed of immune cells (especially lymphocytes) and signalling molecules circulating in blood and lymphatic tissues.
- Main functions:
- Protect against pathogens, tumours, and transplanted tissues
- Achieve this via:
- Direct cellular attacks
- Indirect mechanisms, including chemical messengers and antibodies
Key Terminology
- Pathogen: Disease-causing microorganism
- Pathogenicity: Ability of a microorganism to cause disease
- Virulence: Severity or degree of pathogenicity
- Opportunistic pathogens: Harm normal hosts only when immunity is compromised
- Normal flora: Harmless commensals; can become pathogenic if they breach barriers
- Infection: Breach of physical barriers by microorganisms (including normal flora)
- Disease may not occur if:
- Host immune response is sufficient
- Pathogen load is low
- Entry route is non-threatening
- Disease may not occur if:
Components of the Immune System
| Feature | Innate Immunity | Adaptive Immunity |
|---|---|---|
| Barriers | Skin, mucosa, acid, enzymes | Lymphocyte-lined mucosal barriers |
| Soluble Proteins | Complement, acute-phase proteins | Antibodies |
| Key Cells | Phagocytes, natural killer cells (NKs) | B and T lymphocytes |
| Specificity | Pattern recognition (non-specific) | Highly antigen-specific |
| Memory | Absent | Present |
| Self-tolerance | Present | Present |
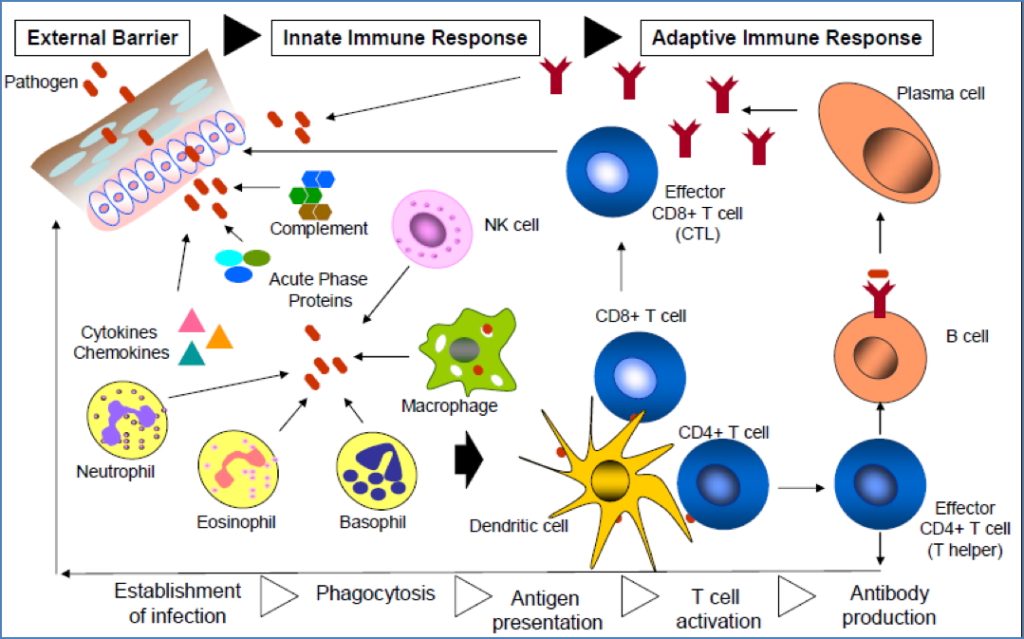
Innate Immune System
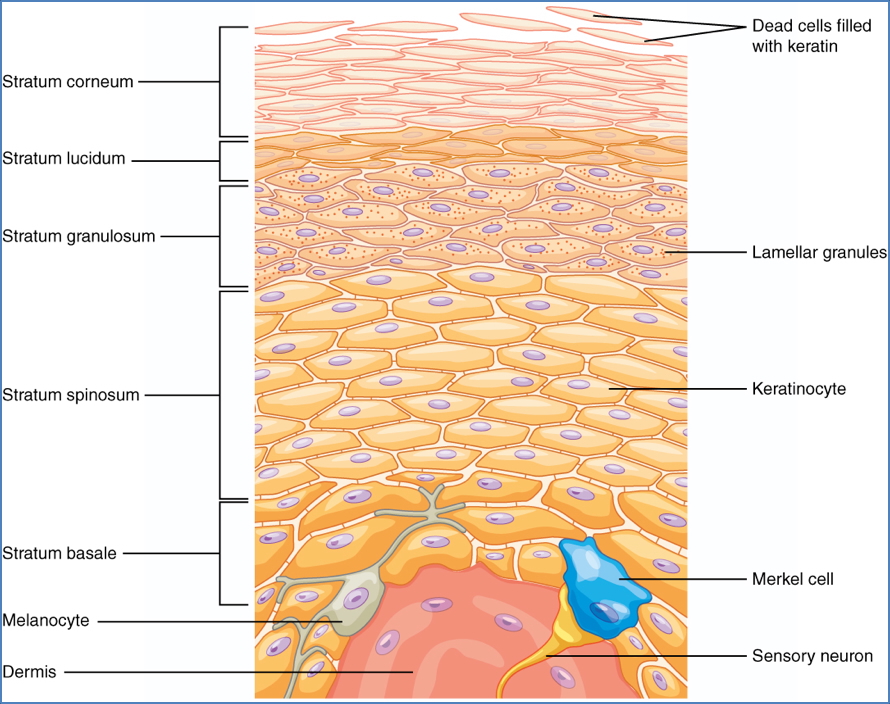
External Barriers (1st Line)
- Skin: Stratified, keratinised barrier
- Mucous membranes:
- Lysozyme (saliva, tears)
- Mucus and cilia (respiratory, GI tracts)
- Acidic secretions (vagina, stomach)
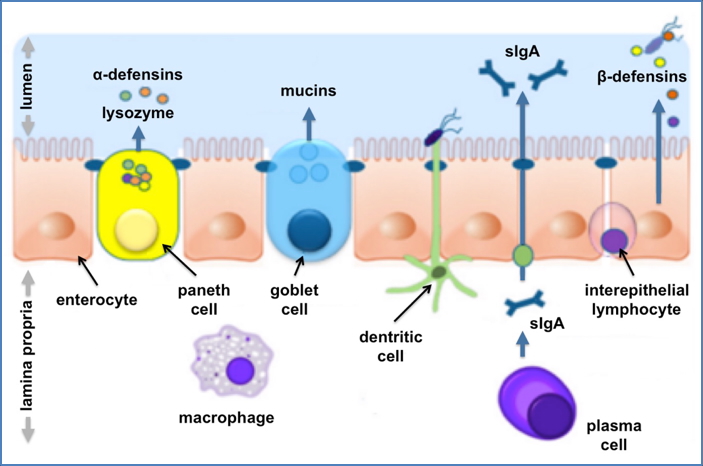
2. Creative Commons: https://commons.wikimedia.org/wiki/File:Bischoff_fig_2.tiff
Internal Defences (2nd Line)
- Phagocytic cells:
- Macrophages: Phagocytose pathogens and debris, present antigens, secrete cytokines
- Neutrophils: Short-lived, highly abundant, form pus

- Granulocytes:
- Eosinophils: Anti-parasitic, mildly phagocytic
- Basophils: Non-phagocytic, mediate allergic reactions

- Natural Killer (NK) cells:
- Target virus-infected and tumour cells
- Kill via apoptosis; secrete pro-inflammatory signals

- Antimicrobial Proteins:
- Interferons: Inhibit viral replication; activate macrophages and NK cells
- Complement system:
- C3b → opsonisation
- MAC → lysis
- C5a → chemotaxis

Complement Cascade and Function The classical pathway, used during adaptive immune responses, occurs when C1 reacts with antibodies that have bound an antigen.
- Fever: Triggered by cytokines (IL-1, IL-6, TNF-α); raises metabolic rate
- Inflammation:
- Triggered by trauma or infection
- Leads to heat, redness, pain, swelling
- Recruits neutrophils, lymphocytes, and macrophages
Adaptive Immune System
- Specific, systemic, and retains memory
- Requires activation via antigen presentation
- Divided into: Cell-Mediated Immunity
- CD8+ cytotoxic T cells → destroy infected or malignant cells
- CD4+ helper T cells → coordinate response via cytokines
- NK cells and macrophages also activated
- B cells produce antigen-specific antibodies
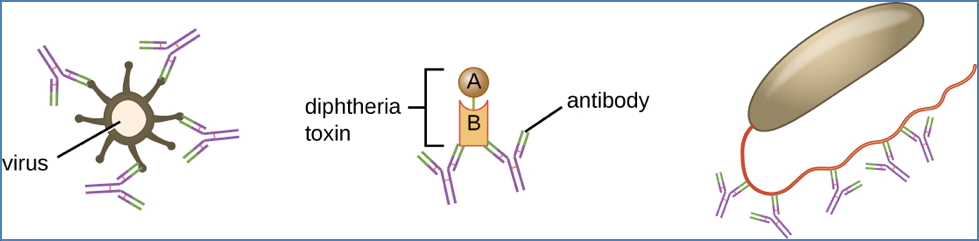
- Antibodies:
- Neutralise pathogens
- Opsonise targets
- Activate complement
- Promote agglutination
- Facilitate antibody-dependent cellular cytotoxicity (ADCC)
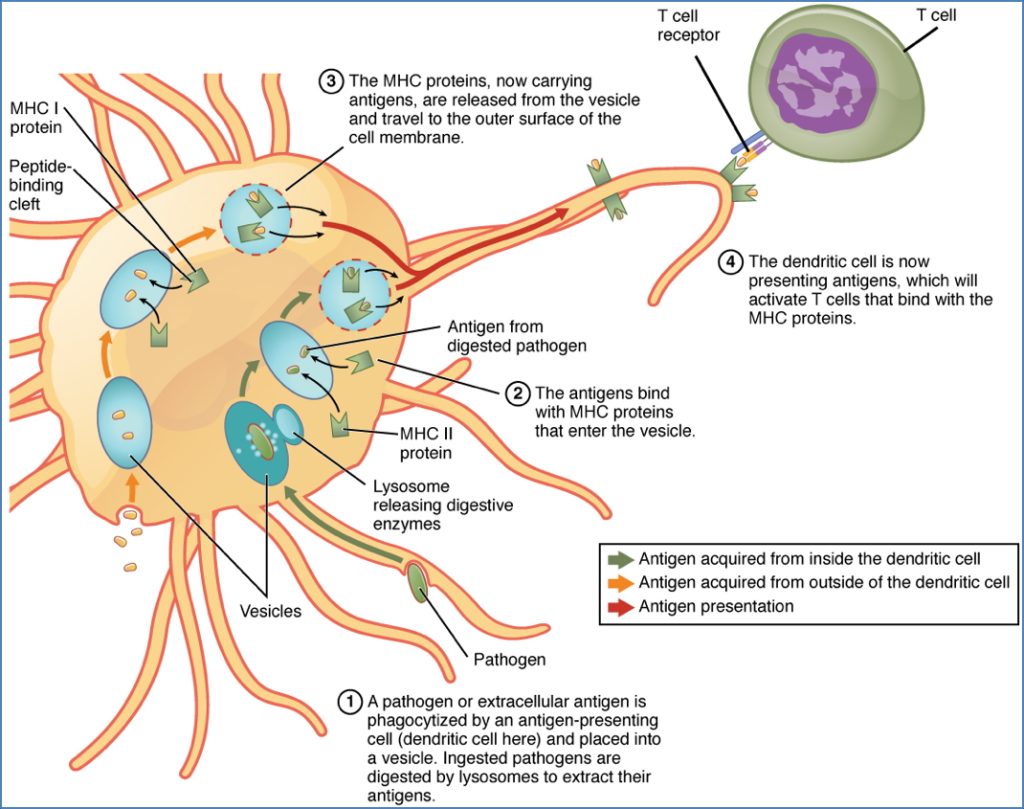
Antigen Presentation
- Performed by Antigen-Presenting Cells (APCs):
- Dendritic cells: Most efficient; activate both CD4+ and CD8+ T cells
- Macrophages: Use MHC-II for T-helper cell activation
- B cells: Present antigen via MHC-II and require CD4+ T-cell help
Antigens and Antibodies
Antigens
- Molecules that bind to B-cell or T-cell receptors
- Immunogens: Trigger antibody production
- Can be:
- Thymus-dependent (require CD4+ help)
- Thymus-independent (activate B cells directly)
- Superantigens: Activate T cells without MHC restriction → cytokine storm
Antibodies (Immunoglobulins)
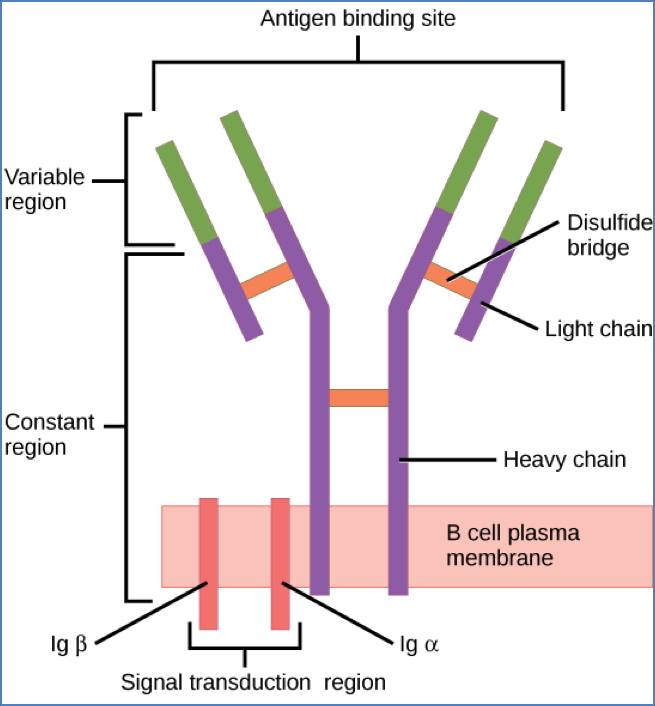
- Structure: Y-shaped, with antigen-binding sites (Fab) and constant region (Fc)
- Found in plasma or on B-cell surfaces
- Isotypes:
- IgM: First produced, activates complement
- IgG: Major serum antibody, crosses placenta
- IgA: Mucosal immunity
- IgE: Allergies and parasites
- IgD: B-cell receptor
Antigen Receptors
B-Cell Receptors (BCRs)
- Surface-bound antibodies (IgM or IgD)
- Bind whole antigens directly
- Capable of isotype switching and affinity maturation
T-Cell Receptors (TCRs)
- Recognise peptide–MHC complexes
- Do not bind free antigen
- αβ or γδ chains define lineage

Pathogen Recognition
Pathogen-Associated Molecular Patterns (PAMPs)
- Conserved microbial features recognised by innate immunity
- Examples:
- LPS (Gram-negative) → TLR-4
- Flagellin → TLR-5
- dsRNA (viruses) → TLR-3
Toll-Like Receptors (TLRs)
- Pattern-recognition receptors on APCs
- Trigger cytokine release, recruit immune cells, and initiate inflammation
Major Histocompatibility Complex
MHC-I
- Found on all nucleated cells
- Presents endogenous peptides to CD8+ T cells
- Enables cytotoxic killing of infected or cancerous cells
MHC-II
- Found only on APCs
- Presents exogenous peptides to CD4+ T cells
- Facilitates B-cell and macrophage activation
MHC Restriction
- TCRs only recognise antigens bound to self-MHC
- Superantigens bypass this → trigger massive T-cell activation → toxic shock

Summary – Immune System Overview
The immune system overview outlines the essential components of host defence, including the innate and adaptive arms. From rapid, non-specific defences like neutrophils and complement to antigen-specific memory via antibodies and cytotoxic T cells, the immune system protects against infection, malignancy, and foreign materials. Understanding antigen presentation, cytokine signalling, and MHC diversity is vital for clinical immunology. For a broader context, see our Immune & Rheumatology Overview page.