Table of Contents
Overview – MHCs
Major Histocompatibility Complexes (MHCs) are cell surface glycoproteins that present antigenic peptides to T-cells. They are essential for T-cell recognition, antigen presentation, and immune activation. MHCs define “self” for the immune system and play a key role in both immunity and transplant rejection. MHC molecules come in two major classes—MHC-I and MHC-II—each with distinct expression profiles and functions.
What Are MHCs?
- Also known as HLA (Human Leucocyte Antigens)
- Encoded by MHC genes on chromosome 6
- Expressed as glycoproteins on cell surfaces
- Enable T-cells to recognise antigen in a restricted, MHC-dependent manner
- Account for transplant rejection due to their extensive genetic polymorphism
- Not expressed on red blood cells
MHC Molecular Structure
MHC Class I
- Expressed on all nucleated cells
- Consists of:
- 1 alpha chain (with 3 domains: α1, α2, α3)
- 1 β2-microglobulin (not MHC-encoded)
- Single intracellular domain
- Binds endogenous peptides (e.g. viral or tumour antigens)
MHC Class II
- Expressed only on APCs: macrophages, dendritic cells, B-cells
- Consists of:
- α-chain and β-chain (both MHC-encoded)
- Two intracellular domains
- Binds exogenous peptides (e.g. phagocytosed pathogens)

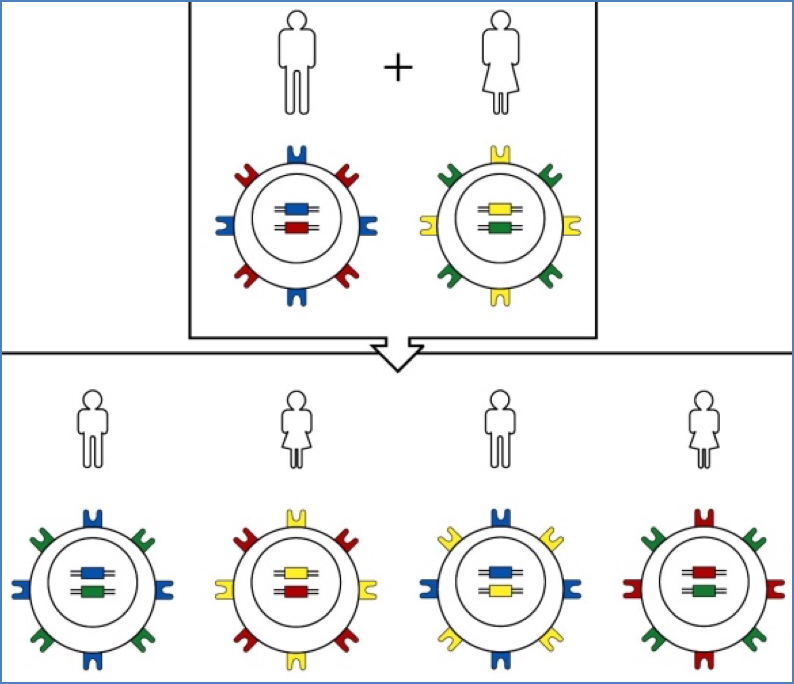
MHC Diversity: Polygeny & Polymorphism
Polygeny
- Multiple genes encode each MHC class
- Class I genes: HLA-A, HLA-B, HLA-C
- Class II genes: HLA-DR, HLA-DP, HLA-DQ
Polymorphism
- Hundreds of alleles exist for each gene
- Expression is co-dominant
- Each person expresses both maternal and paternal alleles
- Basis for MHC-based haplotypes, which are inherited as a unit
- Explains similarity between 1st-degree relatives

MHC-I Functions
- Expressed on all nucleated cells & APCs
- Presents endogenous peptides (e.g. viral proteins)
- Activates CD8+ cytotoxic T-cells
- Enables thymic selection of CD8+ T-cells
- Allows cytotoxic targeting of cancerous or infected cells

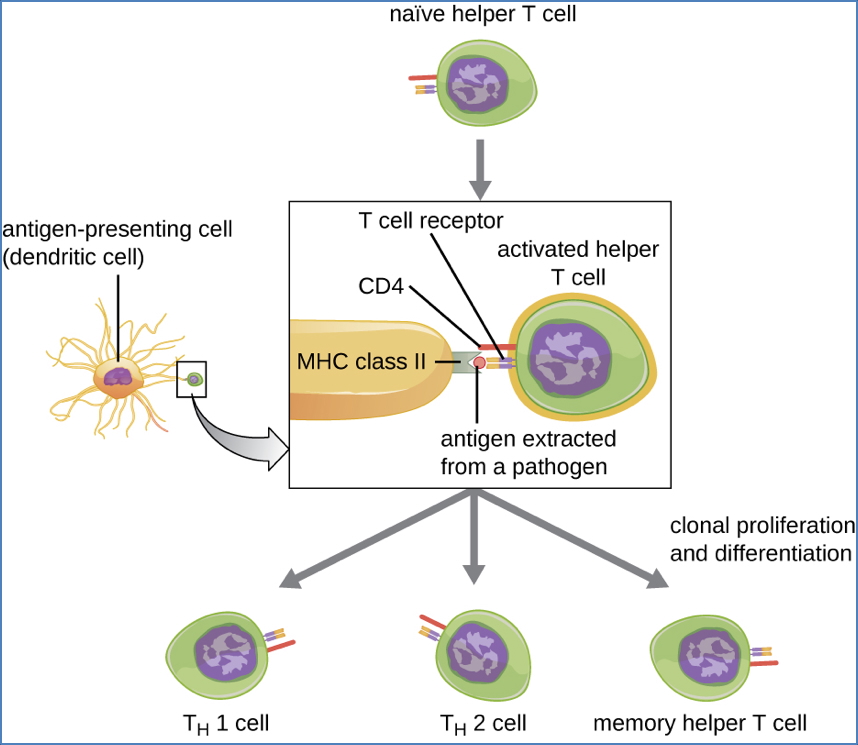
MHC-II Functions
- Expressed only on APCs, semi-activated macrophages, and B-cells
- Presents exogenous peptides (e.g. phagocytosed pathogens)
- Activates CD4+ helper T-cells
- Required for:
- Thymic selection of CD4+ T-cells
- TH-cell help to activate macrophages and B-cells
- Isotype switching and antibody secretion by B-cells
Antigen Processing & MHC Presentation
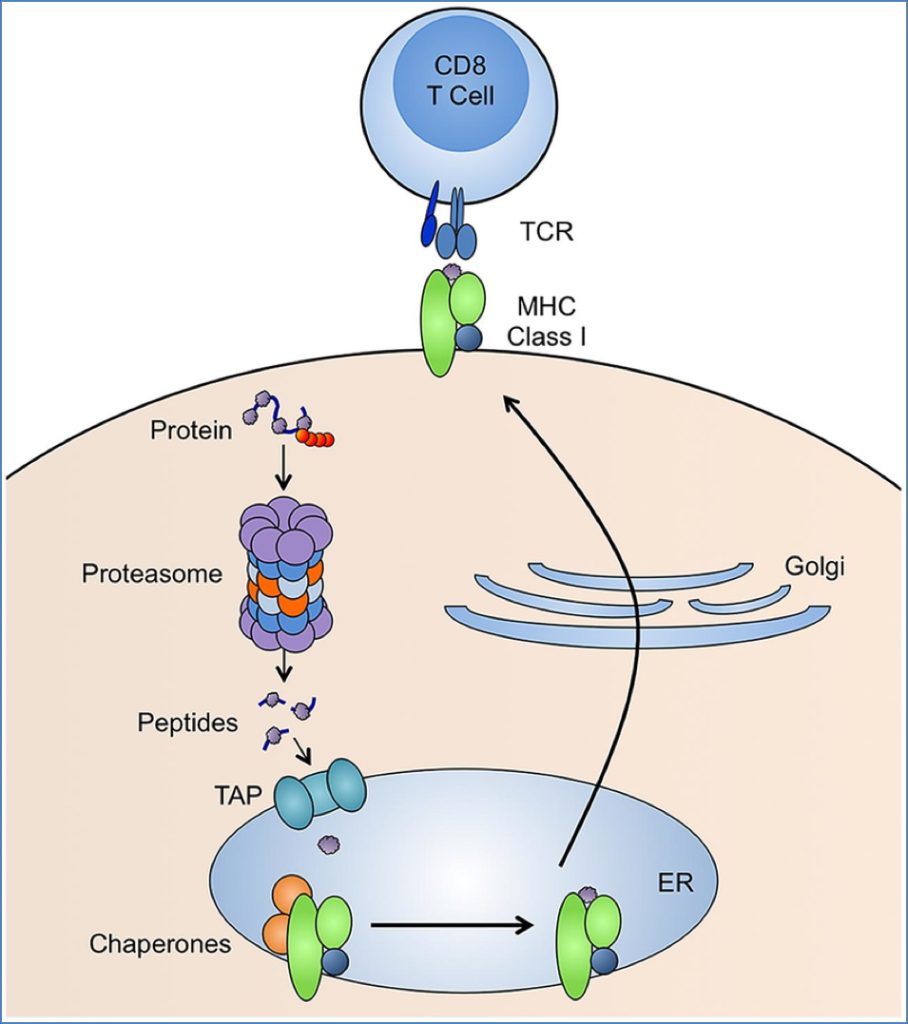
MHC-I Pathway (Endogenous Ags)
- Cytosolic antigens (e.g. viruses, mutated proteins)
- Degraded by proteasomes → peptide fragments
- Peptides transported into ER via TAP transporters
- Peptides loaded onto MHC-I (chaperones assist)
- pMHC-I transported to cell surface
- Recognised by CD8+ T-cells
Clinical Note:
- Some viruses & TAP mutations can disrupt this pathway to evade immunity
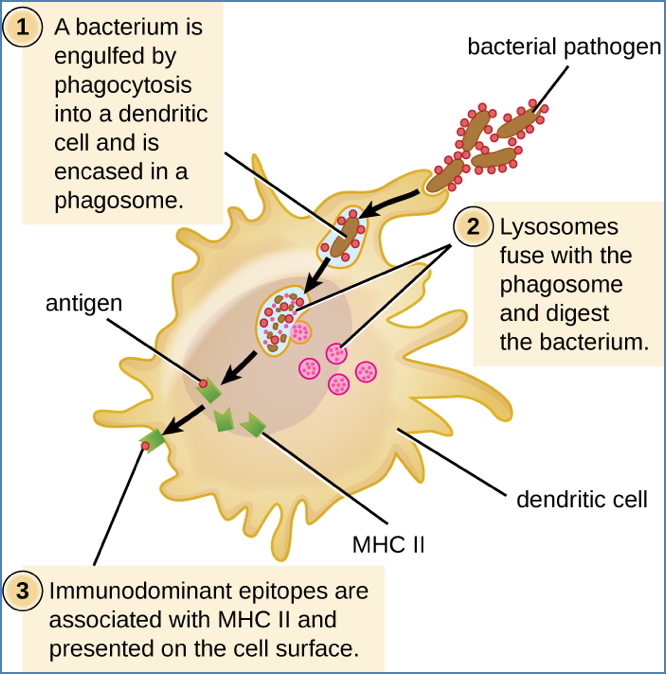
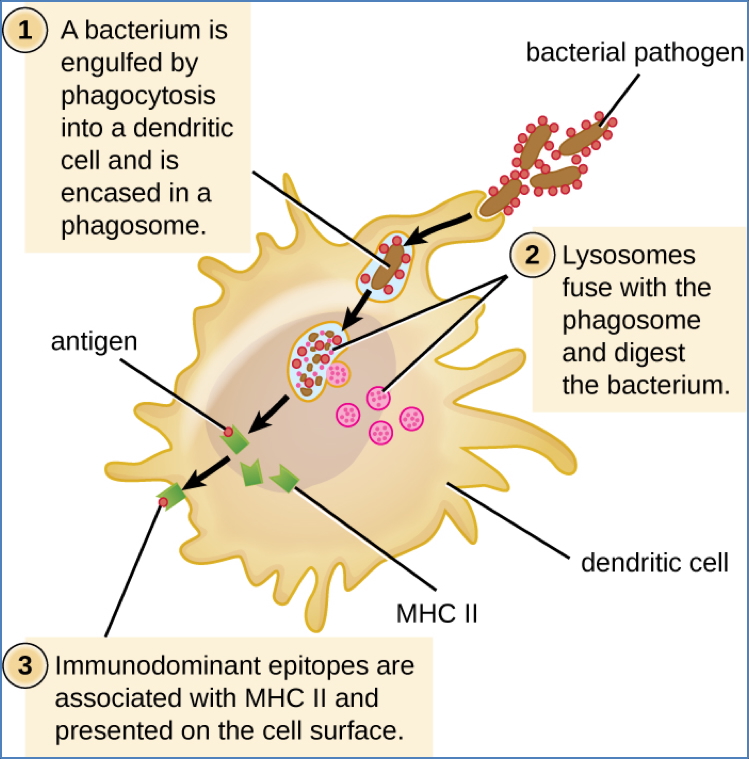
MHC-II Pathway (Exogenous Ags)
- Extracellular antigens are phagocytosed
- Phagosome fuses with lysosome → phagolysosome
- Acid degrades antigen → peptide fragments
- MHC-II molecules carry CLIP (invariant chain) to block premature peptide binding
- In lysosome, HLA-DM removes CLIP → peptide loaded onto MHC-II
- pMHC-II transported to surface for CD4+ T-cell recognition
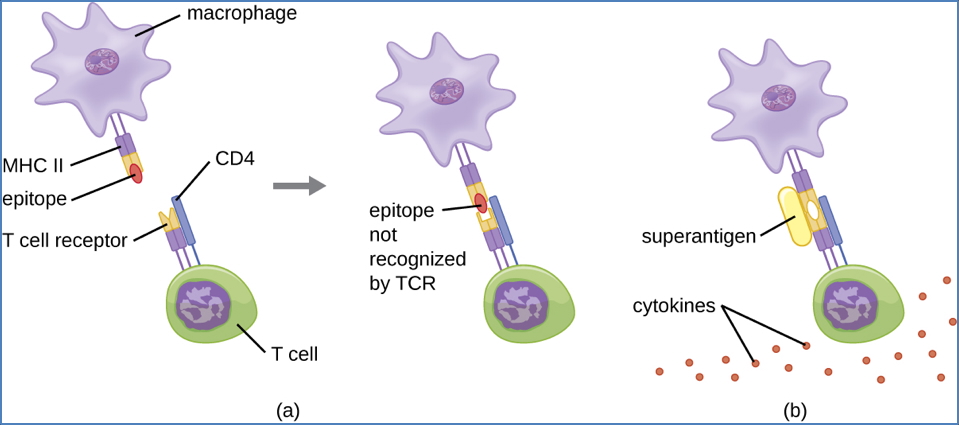
MHC Restriction
- T-cell receptors (TCRs) only recognise antigen when presented with self MHC
- Two conditions must be met:
- Compatible MHC molecule
- Specific antigenic peptide
- Prevents inappropriate immune activation
- Basis for “self vs non-self” immune recognition
Superantigens
- Bacterial/viral antigens that bypass MHC restriction
- Bind outside the MHC-TCR cleft → trigger non-specific T-cell activation
- Lead to cytokine storm → ↑↑ IL-2, TNF-α, IFN-γ → Toxic Shock Syndrome
Clinical Features
- Fever, hypotension, tachycardia
- Myalgia, dizziness, rash
Management
- Aggressive antibiotic/antiviral therapy
- Symptomatic support
Summary – MHCs
MHCs are glycoproteins that present antigen to T-cells, enabling immune surveillance, thymic selection, and T-cell activation. MHC Class I presents endogenous antigens to CD8+ T-cells, while MHC Class II presents exogenous antigens to CD4+ T-cells. Their extreme polymorphism underpins transplant rejection and immune diversity. For more immunological concepts, visit our Immune & Rheumatology Overview.