Table of Contents
Overview – Colorectal Cancer
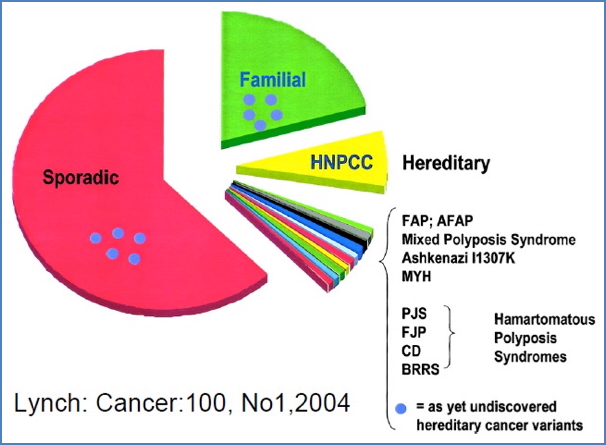
Colorectal cancer (CRC) is a malignant tumour arising from the epithelium of the colon or rectum, typically originating from pre-cancerous adenomatous polyps. It is one of the most common cancers in the Western world, with a prevalence of approximately 4%. While most cases are sporadic, some are inherited—particularly familial adenomatous polyposis (FAP) and hereditary non-polyposis colorectal cancer (HNPCC). Early detection is critical, as CRC often progresses silently until symptoms emerge. Screening, genetics, and lifestyle modification play essential roles in prevention and prognosis.
Definition
- Malignancy of the colon or rectum due to excess replication of stem cells in colonic crypts
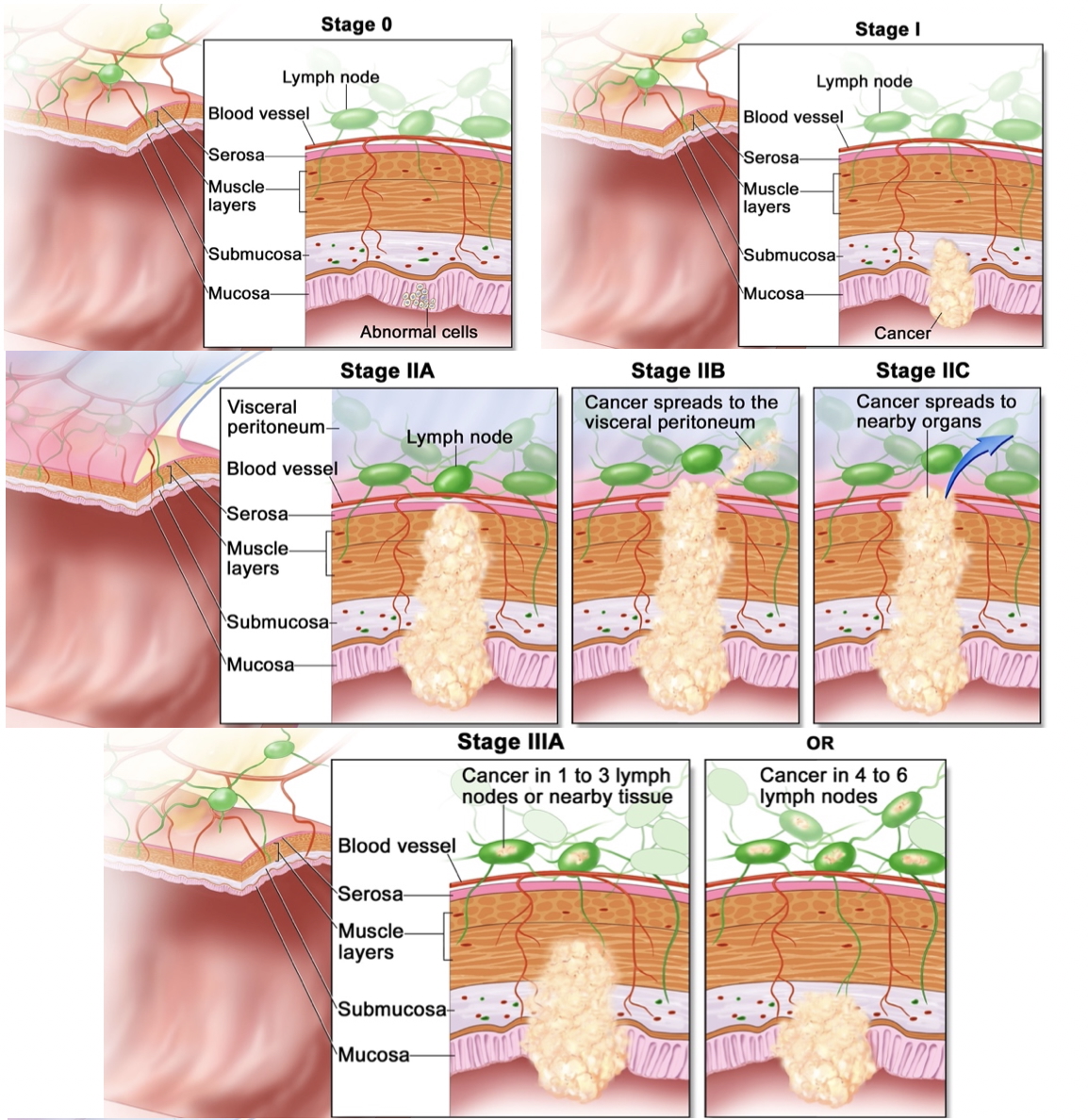
- Progresses from benign polyps → dysplastic lesions → invasive carcinoma
- Commonly classified using Duke’s staging (A–D) or Stage 0–4 system
Aetiology
Sporadic vs Inherited
- Sporadic CRC:
- No clear genetic predisposition
- Typically affects the descending (distal) colon
- Inherited CRC:
- Autosomal dominant
- Typically affects the ascending (proximal) colon
Risk Factors
- Age > 50 years (≈90% of CRCs diagnosed in this group)
- Colorectal polyps (especially adenomas)
- Family history (30% of CRCs are hereditary)
- HNPCC → 70–80% lifetime risk
- FAP → 95–100% lifetime risk
- Inflammatory bowel disease (Crohn’s, ulcerative colitis)
- Diet: high fat, low calcium, low folate, low fibre
- Smoking
Clinical Features
- Often asymptomatic in early stages
- Change in bowel habits: diarrhoea, constipation
- Altered stool shape: ribbon-like stools from partial obstruction
- Abdominal cramping and bloating
- Intermittent bleeding:
- Can result in iron-deficiency anaemia
- Detected by faecal occult blood test (FOBT)
- Unexplained weight loss, fatigue, anorexia
Pathogenesis
- Progresses via the adenoma–carcinoma sequence:
- Hyperproliferation →
- Adenomatous polyps (small → large) →
- Severe dysplasia (pre-cancerous) →
- Adenocarcinoma
- Adenomas often have a villous component
- Histologically: dysplastic, anaplastic, rapidly proliferative

Genetics of Colorectal Cancer
1. Familial Adenomatous Polyposis (FAP)
- Autosomal dominant
- Caused by mutation in APC tumour suppressor gene
- Hundreds–thousands of adenomatous polyps
- 90%+ benign but too numerous to manage individually
- Attenuated FAP = fewer polyps (~30)
- Increased risk of other extra-colonic cancers


2. Samir at the English-language Wikipedia, CC BY-SA 3.0 <http://creativecommons.org/licenses/by-sa/3.0/>, via Wikimedia Commons
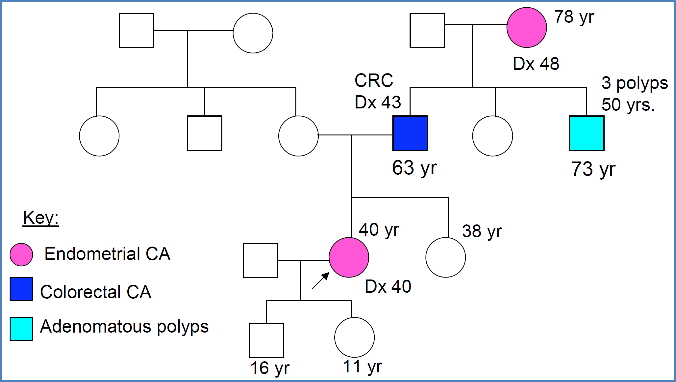
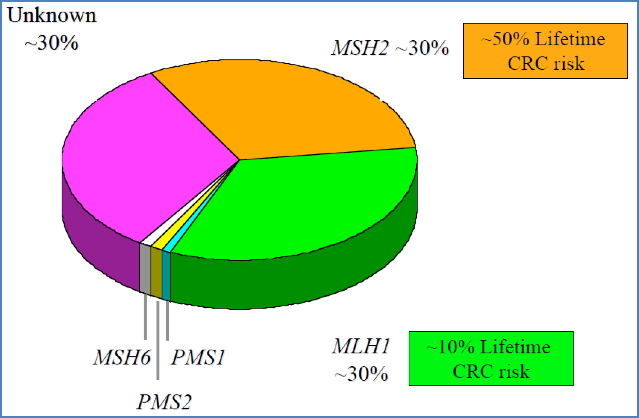
2. Hereditary Non-Polyposis Colorectal Cancer (HNPCC)
- Autosomal dominant
- Caused by mutations in MMR (Mismatch Repair) genes:
- MSH2 (~30%)
- MLH1 (~30%)
- ~30% remain genetically unexplained
- Few adenomas, but synchronous/metachronous polyps common
- Associated with other cancers: endometrial, gastric, ovarian etc.
- Diagnosis requires meeting the Amsterdam II Criteria:
- ≥3 relatives with HNPCC-associated cancers
- ≥1 first-degree relative of the others
- ≥2 successive generations affected
- ≥1 diagnosis before age 50

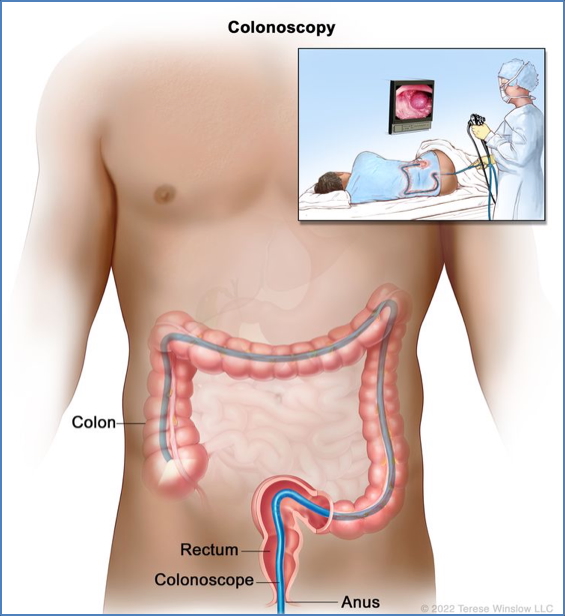
Investigations
- Colonoscopy = gold standard
- Faecal Occult Blood Test (FOBT) = for screening
- Biopsy = histological confirmation
- Genetic testing if family history is suggestive of HNPCC or FAP

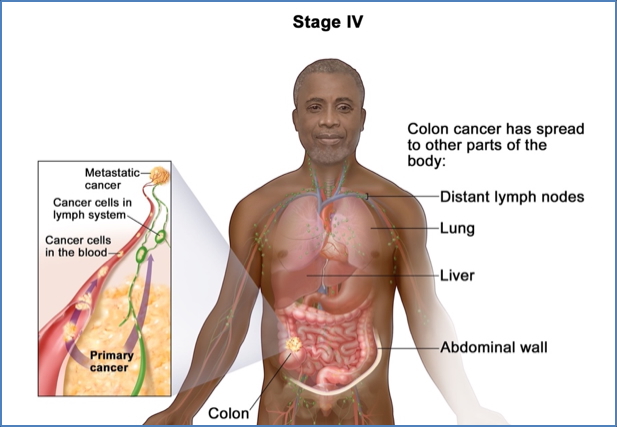
Staging
Duke’s Staging

Numbered Staging

Management
Surgical
- Proximal tumours: resection + anastomosis
- Rectal tumours: resection + possible colostomy


Preventive
- Screening colonoscopy every 1–2 years
- Start at 25 years old or 5 years earlier than youngest family diagnosis
- Genetic counselling and testing in hereditary cases
Complications
- Obstruction
- Perforation
- Metastasis (especially to liver, lungs)
- Anaemia from chronic blood loss
- Recurrence after surgical resection
Summary – Colorectal Cancer
Colorectal cancer is a prevalent malignancy that progresses from benign polyps to invasive carcinoma, with risks increased by age, genetic predisposition, and lifestyle factors. FAP and HNPCC represent key inherited syndromes linked to mutations in APC and mismatch repair genes, respectively. Early detection through colonoscopy and FOBT is crucial for favourable outcomes. For a broader context, see our Genetics & Cancer Overview page.