Table of Contents
Overview – Acute Lymphoblastic Leukaemia
Acute Lymphoblastic Leukaemia (ALL) is a malignant proliferation of immature lymphoid precursors (lymphoblasts), most commonly affecting children aged 4–5. It is the most common paediatric cancer and, with timely treatment, has a favourable prognosis. If untreated, it can progress rapidly and be fatal within weeks to months. This article outlines the key clinical features, diagnostic criteria, and management essentials for final-year medical exams.
Definition
- A malignant clonal expansion of lymphoblasts in the bone marrow
- Results in bone marrow failure, systemic infiltration, and immunosuppression
- Most commonly of B-cell lineage
Aetiology
- Multifactorial, involving:
- Genetic predispositions (e.g. Down syndrome, ataxia-telangiectasia)
- Chromosomal translocations (e.g. Philadelphia chromosome t(9;22))
- Environmental triggers: ionising radiation, viral infections
Pathophysiology
- Mutation in lymphoid progenitor cells →
- Uncontrolled proliferation of B-lymphoblasts (or less commonly, T-lymphoblasts)
- Suppression of normal haematopoiesis → Anaemia, neutropenia, thrombocytopenia
- Infiltration of organs (e.g. liver, spleen, CNS, lymph nodes)
Clinical Features
- Demographics: Most common in children (4–5 years), slight male predominance
- Symptoms:
- Bone pain (often sternum, long bones)
- Fatigue, pallor (from anaemia)
- Easy bruising, petechiae (from thrombocytopenia)
- Fever, recurrent infections (from neutropenia)
- Weight loss, anorexia
- General malaise
- Signs:
- Lymphadenopathy (cervical, axillary, mediastinal)
- Hepatosplenomegaly
- Oedema (esp. lower limbs if venous/lymphatic obstruction)
Investigations
- FBC:
- ↓ Hb
- ↓ Platelets
- Often ↑ WCC (but may be normal or low)
- Blast cells visible
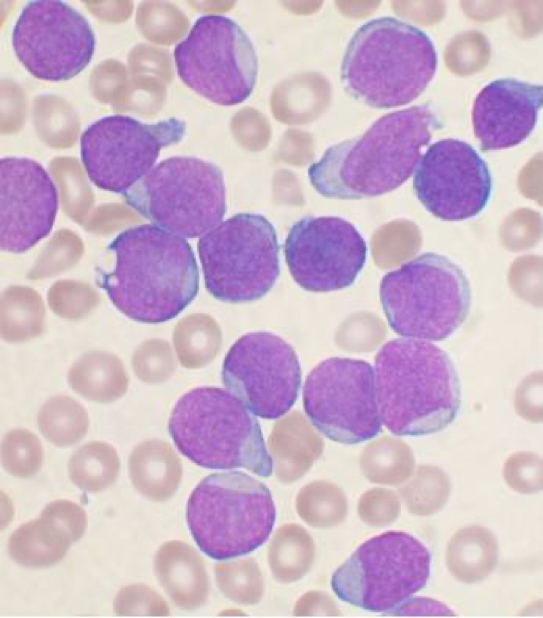
- Blood film:
- Lymphoblasts (large cells with scant cytoplasm and large nuclei)
- Bone marrow biopsy:
- 20% lymphoblasts required for diagnosis
- Cytogenetics:
- Identify chromosomal abnormalities
- Look for Philadelphia chromosome (especially in adults)
- Cytochemistry:
- Myeloperoxidase & Sudan Black staining → NEGATIVE in ALL (helps differentiate from AML)
- Imaging:
- CXR → mediastinal mass (especially in T-ALL)
- CT/MRI if CNS involvement suspected
- Lumbar puncture:
- Assess for CNS infiltration
Management
- Supportive care:
- Blood transfusions, platelets
- Antimicrobials (IV antibiotics, antifungals, antivirals)
- Tumour lysis prophylaxis (allopurinol, hydration)
- Chemotherapy:
- Induction → Consolidation → Maintenance phases
- CNS prophylaxis (intrathecal methotrexate)
- Bone marrow transplant:
- Reserved for high-risk or relapsed cases
Prognosis
- Paediatric ALL: Excellent (70–90% cure rates)
- Prognostic factors:
- Age (1–10 years better)
- WCC at diagnosis (<50,000 favourable)
- Cytogenetics (t(12;21) = favourable; t(9;22) = poor)
Summary – Acute Lymphoblastic Leukaemia
Acute Lymphoblastic Leukaemia (ALL) is the most common childhood cancer and is defined by malignant proliferation of lymphoblasts. It presents with bone marrow failure, lymphadenopathy, and systemic symptoms. Diagnosis is confirmed via bone marrow biopsy and cytogenetic testing. With modern chemotherapy regimens and supportive care, the majority of paediatric patients achieve long-term remission. For more on blood disorders, see our Blood & Haematology Overview page.