Table of Contents
Overview – Haemolytic Anaemia
Haemolytic anaemia refers to a group of conditions in which red blood cells are destroyed prematurely, leading to anaemia, jaundice, and elevated bilirubin. It may occur via extravascular mechanisms (e.g. splenic macrophage destruction) or intravascular processes (e.g. haemoglobinaemia and haemoglobinuria). Common causes include autoimmune disease, hereditary membrane defects, enzyme deficiencies, haemoglobinopathies, and mechanical trauma. A clear diagnostic approach is essential for identifying the underlying cause and directing appropriate treatment.
Definition
- Anaemia caused by increased destruction of red blood cells (RBCs)
- Can occur intravascularly (within blood vessels) or extravascularly (in spleen/liver)
- Results in release of free haemoglobin, hyperbilirubinaemia, and reticulocytosis
Aetiology
Intravascular Haemolysis
- Paroxysmal Nocturnal Haemoglobinuria (PNH)
- Severe infections (e.g. malaria)
- Mechanical destruction (e.g. prosthetic valves, DIC)
- Transfusion reactions (ABO mismatch)
Extravascular Haemolysis
- Occurs in reticuloendothelial system (spleen, liver)
- May be due to:
- Autoimmune haemolytic anaemia (AIHA)
- Enzyme defects (e.g. G6PD deficiency)
- Membrane defects (e.g. hereditary spherocytosis)
- Haemoglobinopathies (e.g. thalassaemia, sickle cell)
- Drugs/toxins
- Hypersplenism

Pathophysiology
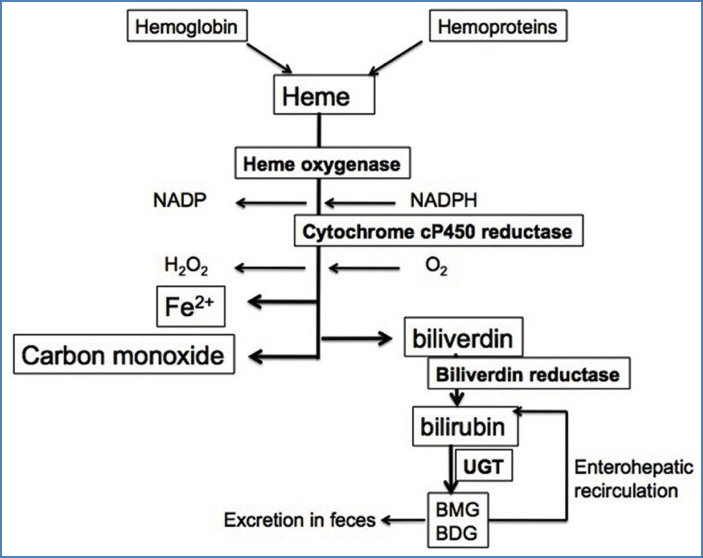
- RBC destruction → free haemoglobin released into plasma
- Heme → protoporphyrin + iron
- Protoporphyrin → unconjugated bilirubin → causes jaundice
- Bilirubin is conjugated in liver → excreted in bile/faeces
- Chronic haemolysis may → gallstones and iron overload
Clinical Features
Symptoms
- General anaemia symptoms (fatigue, dyspnoea)
- Jaundice (mild, fluctuating)
- Dark urine (haemoglobinuria)
- Splenomegaly
- Venous stasis ulcers (e.g. in sickle cell)
- Raynaud’s phenomenon (in cold agglutinin disease)
Investigations
Laboratory Findings
- ↓ Hb
- ↑ Reticulocyte count
- ↑ LDH
- ↑ Unconjugated bilirubin
- ↓ Haptoglobin
- Haemoglobinaemia, haemoglobinuria, haemosiderinuria
Blood Film
- Evidence of:
- Reticulocytosis
- Broken/fractured RBCs
- Target cells, spherocytes, bite cells (depending on cause)

Specific Tests
- Direct Coombs (DAT): positive in autoimmune causes
- G6PD screen
- Sickle cell test / Hb electrophoresis
- Bone marrow biopsy (rarely needed)
Diagnostic Approach – 4Q Method
- Is there increased RBC breakdown?
- Jaundice, ↑ Urobilinogen
- Is there increased RBC production?
- ↑ Reticulocytes, polychromasia, ↑ MCV
- Where is haemolysis occurring?
- Intravascular → haemoglobinaemia, haemoglobinuria
- Extravascular → splenomegaly
- Why is there haemolysis?
- Autoimmune (WAHA, CAHA) → positive Coombs
- Congenital (sickle, thalassaemia, G6PD) → abnormal film
- Mechanical (DIC, valve, MAHA) → schistocytes
Treatment
- Treat underlying cause
- Immunosuppression or plasmapheresis if autoimmune
- Splenectomy for hereditary spherocytosis or hypersplenism
- Transfusions if severe anaemia
- Folic acid supplementation
- Vaccination and prophylaxis post-splenectomy
Summary – Haemolytic Anaemia
Haemolytic anaemia is caused by premature destruction of red blood cells, either intravascularly or extravascularly. It presents with anaemia, jaundice, splenomegaly, and signs of haemolysis on lab tests. Diagnosis requires careful evaluation of blood film, haemolysis markers, and autoimmune screening. Treatment depends on the cause, ranging from immunosuppressive therapy to splenectomy. For a broader context, see our Blood & Haematology Overview page.