Table of Contents
Overview – Thrombotic Disorders
Thrombotic disorders refer to inappropriate clot formation within blood vessels due to excessive activation of the clotting cascade or impaired anticoagulant control. These clots—composed of platelets and fibrin—can obstruct blood flow, cause tissue ischaemia, or embolise to distant sites. They underlie many serious clinical conditions, including pulmonary embolism, stroke, and myocardial infarction. Understanding their mechanisms is essential for effective prevention and treatment.
Definition
- Thrombosis = Inappropriate formation of fibrin and platelet clots
- Leads to vascular obstruction → Ischaemia → Necrosis
- Thromboembolism = A clot that dislodges and migrates to another site (e.g. DVT → PE)
Arterial Thrombosis
Mechanisms:
- Atherosclerotic Plaque Rupture
- Rupture exposes subendothelial collagen & tissue factor
- → Triggers platelet aggregation & coagulation → Thrombosis
- Thromboembolism
- E.g. Atrial fibrillation → clot in left atrium → embolises to brain → Stroke
Risk Factors:
- Age
- Male sex
- Hypertension
- Diabetes
- Smoking
- Hyperlipidaemia
- Obesity
- Family history
Common Presentations:
- Stroke (CVA)
- Myocardial infarction (MI)
- Peripheral Arterial Disease (PAD)
Venous Thrombosis
Sites:
- Commonly in lower limbs (gravity-dependent venous pooling)
- Deep & superficial veins
- May lead to Pulmonary Embolism (PE)
Risk Factors:
Hereditary Hypercoagulable States:
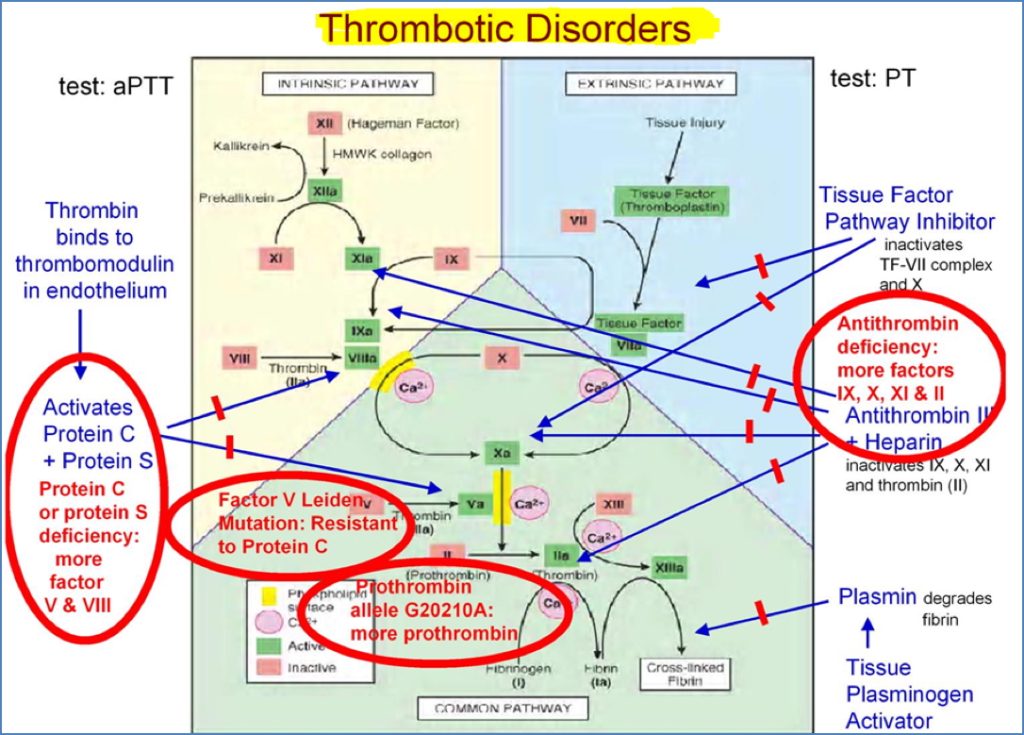
- Factor V Leiden mutation
- Prothrombin G20210A variant
- Protein C/S deficiency
- Antithrombin III deficiency
Acquired Hypercoagulable States:
- High-dose oestrogen therapy (↑Coagulation factors, ↓Antithrombin)
- Surgery/trauma (tissue factor exposure + immobility)
- Pregnancy/post-partum
- Sepsis
- Heparin-induced thrombocytopenia (HIT)
- Venous stasis due to:
- Heart failure
- Stroke
- Prolonged immobility
- Nephrotic syndrome
- Varicose veins
Treatment:
- Anticoagulants (oral or parenteral)
- Haemodynamic support
- Endovascular clot retrieval (in severe cases)
Complications
- Pulmonary embolism
- 95% originate from leg/calf DVTs
- Causes ischaemia or infarction of lung tissue
- Post-thrombotic syndrome
- Chronic venous insufficiency


2.https://www.scientificanimations.com, CC BY-SA 4.0 <https://creativecommons.org/licenses/by-sa/4.0>, via Wikimedia Commons
Evaluation of Thrombotic Disorders
Indications for Thrombophilia Screening:
- Family history
- Unprovoked thrombosis at a young age
- Recurrent DVT
- Unusual sites (e.g. cerebral, hepatic, mesenteric veins)
Initial Workup:
- FBC + ESR
- Changes in platelets, haematocrit, fibrinogen
- Evidence of haemolysis or inflammation
- Prothrombin Time (PT)
- Detects Factor VII deficiency
- Reflects extrinsic pathway
- Activated Partial Thromboplastin Time (aPTT)
- Detects Factors VIII, IX, XI, XII deficiencies
- Reflects intrinsic pathway
- INR
- Used to monitor warfarin therapy
- Detects inadequate anticoagulation
If Both PT & aPTT Abnormal → Consider:
- Liver disease
- Vitamin K deficiency
- Oral anticoagulant toxicity
Summary – Thrombotic Disorders
Thrombotic disorders involve pathological clot formation within arteries or veins and can present as life-threatening events such as strokes, myocardial infarctions, or pulmonary emboli. Evaluation includes a detailed history, risk factor assessment, and lab testing (e.g. PT, aPTT, INR). Understanding underlying mechanisms is essential for guiding prevention and therapy. For broader haematological context, visit our Blood & Haematology Overview page.