Table of Contents
Overview – Acute Coronary Syndromes
Acute coronary syndromes (ACS) refer to a spectrum of clinical presentations caused by acute myocardial ischaemia due to rupture of an unstable atheromatous plaque. These include non-ST-elevation myocardial infarction (NSTEMI), ST-elevation myocardial infarction (STEMI), and unstable angina. Prompt recognition and intervention are critical to prevent extensive myocardial necrosis and reduce mortality.
Definition
- Acute Coronary Syndrome (ACS) includes:
- Unstable Angina
- NSTEMI – Non-ST-elevation myocardial infarction
- STEMI – ST-elevation myocardial infarction
Aetiology
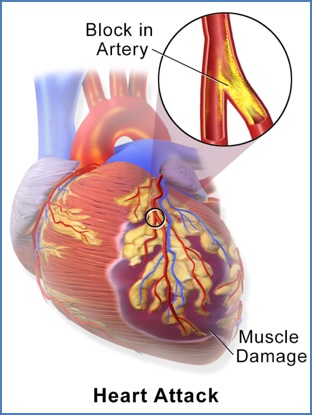
- Caused by rupture of an unstable atheromatous plaque within the coronary arteries.
- May lead to prolonged ischaemia and myocardial necrosis.
Pathogenesis
- Plaque rupture → platelet aggregation + thrombus → acute coronary occlusion
- Results in:
- Sudden cardiac death
- Acute systolic dysfunction/heart failure
- Ventricular rupture
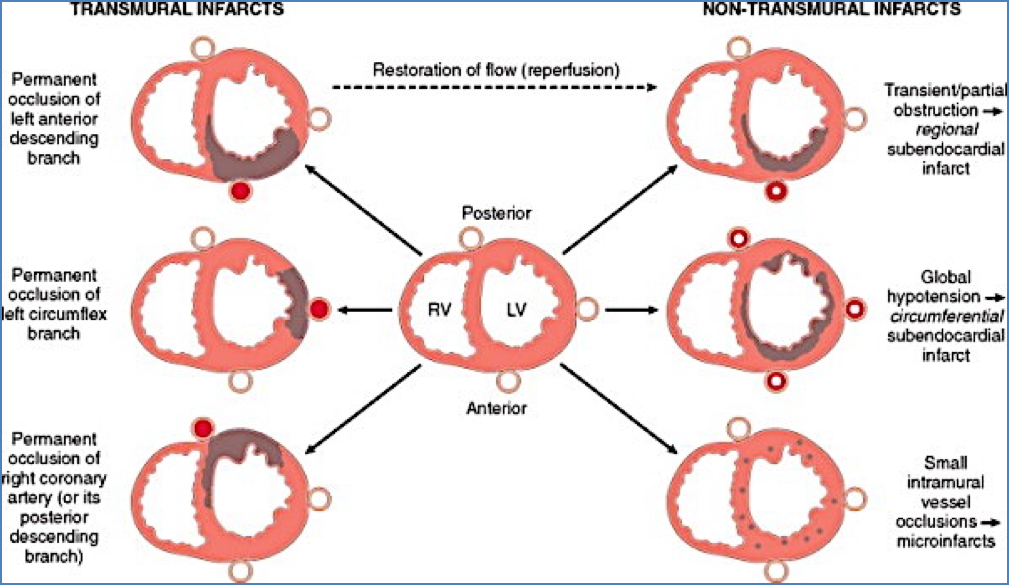
- Progression of ischaemic necrosis:
- Subendocardial Necrosis → NSTEMI:
- ST-depression + T-wave inversion
- Transmural Necrosis → STEMI:
- ST-elevation + T-wave inversion + pathological Q-waves
- Endocardium usually spared due to perfusion from ventricular cavity
- Subendocardial Necrosis → NSTEMI:
Common Sites of Coronary Occlusion
- Left Anterior Descending (LAD) artery – 50%
- Anterior LV, apex, anterior 2/3 of interventricular septum
- Right Coronary Artery (RCA) – 30%
- Posterior LV, posterior septum, right ventricular free wall
- Left Circumflex Artery (LCX) – 20%
- Lateral LV (excluding apex)
- Nearly all infarcts involve some portion of the left ventricle
Clinical Features
Symptoms
- >20 minutes of central, crushing chest pain radiating to:
- Arms
- Neck
- Jaw
- Often accompanied by:
- Dyspnoea
- Nausea
- Feeling of impending doom
- Note: Silent presentations common in:
- Diabetics
- Post-operative patients
- Elderly
Signs
- Sympathetic drive: diaphoresis
- Hypotension: cool peripheries, thready pulse
- Pulmonary congestion: tachypnoea, raised JVP
- May show signs of peripheral vascular disease (PVD)
Investigations
1st Line
- Serial 12-lead ECGs (every 15 minutes initially):
- ST-changes localise infarct:
- V1–V4: Anterior MI
- II, III, aVF: Inferior MI
- I, aVL, V5–V6: Lateral MI
- ST-changes localise infarct:
- Cardiac telemetry – for arrhythmia monitoring
- Serial troponin I/T or CK-MB:
- At presentation, 6 hours, and within 24 hours
- Routine bloods: FBC, U&Es, glucose, lipids
2nd Line
- Transthoracic/transoesophageal echocardiography (TTE/TOE):
- Assess ventricular function
- Rule out differentials (e.g. aortic dissection, pericarditis, PE)
- Myocardial perfusion scanning (nuclear medicine):
- Defines location and extent of infarct
Management
Initial Emergency Management (MONA):
- Morphine – for pain relief and vasodilation
- Oxygen – if hypoxic
- Nitrates – GTN or isosorbide mononitrate
- Aspirin – antiplatelet
Medical Maintenance Therapy
- Anti-anginals
- Nitrates (GTN, isosorbide mononitrate)
- β-blockers (e.g. metoprolol, propranolol)
- Calcium channel blockers (e.g. nifedipine, verapamil)
- Antiplatelet therapy
- Aspirin and/or clopidogrel
- Statins
- Atorvastatin or simvastatin
- Anticoagulation
- Heparin, low molecular weight heparin (LMWH), or warfarin
Definitive Treatment – Revascularisation
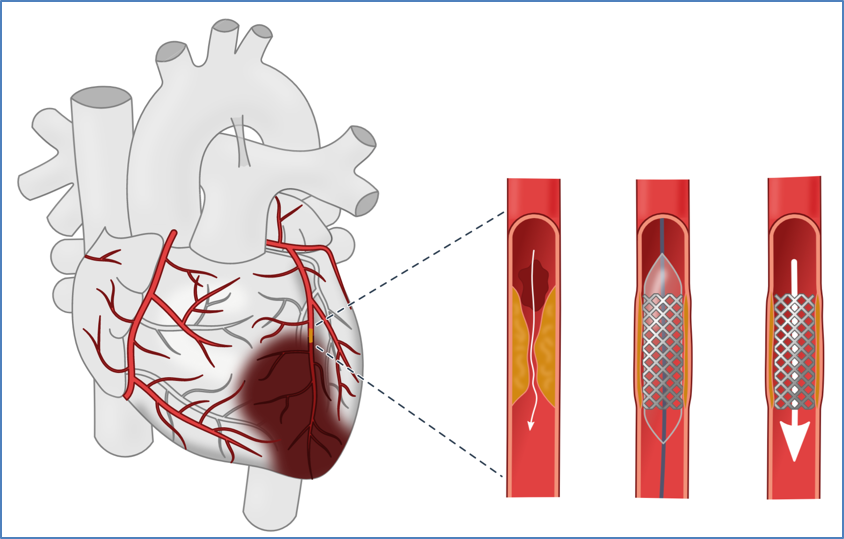
- Percutaneous Coronary Intervention (PCI) – within 4 hours
- Balloon angioplasty and stent placement
- Thrombolysis (e.g. Alteplase/TPA) – if PCI not available
- Contraindications: recent stroke, aortic dissection, active bleeding
- Coronary Artery Bypass Graft (CABG) – in select cases
Complications
Acute
- Left ventricular failure → pulmonary oedema, cardiogenic shock
- Life-threatening arrhythmias: ventricular tachycardia (VT), ventricular fibrillation (VF)
- Myocardial rupture → cardiac tamponade or ventricular septal defect (VSD)
- Mural thrombus → embolism → stroke
Chronic
- Ventricular aneurysm
- Papillary muscle rupture → mitral regurgitation
- Chronic congestive cardiac failure (CCF)
Summary – Acute Coronary Syndromes
Acute coronary syndromes represent a spectrum of myocardial ischaemia due to plaque rupture and thrombotic coronary artery obstruction, leading to NSTEMI or STEMI. Clinical features include prolonged chest pain, ECG changes, and raised troponin. Management involves emergency intervention (MONA), antithrombotic therapy, and definitive revascularisation. Early recognition and treatment are essential to prevent complications like arrhythmias, heart failure, or death. For broader context, see our Cardiovascular Overview page.