Table of Contents
Overview – Cardiac Cycle Physiology
Cardiac cycle physiology describes the mechanical and electrical events that occur during one complete heartbeat. These events include atrial contraction, ventricular contraction (systole), and relaxation (diastole), and are tightly linked to pressure and volume changes within the chambers. A clear understanding of the cardiac cycle is essential for interpreting heart sounds, ECG timing, cardiac output, and the pathophysiology of conditions like heart failure and valvular disease.
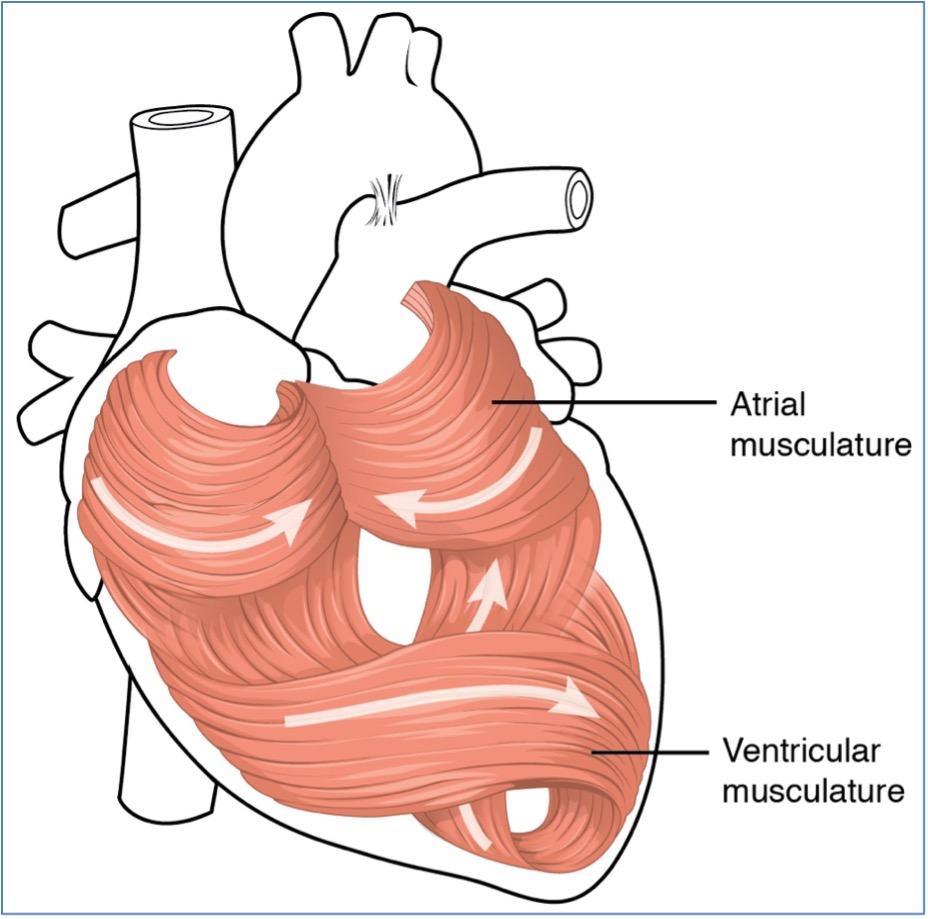
Structure–Function Relationship of the Heart
- The myocardium is arranged in a spiral-like orientation
- Facilitates electrical integration of the heart
- Enables an efficient wringing motion that maximises blood ejection
- Supports strong, coordinated pumping
Key Definitions
- Systole = Myocardial contraction
- Diastole = Myocardial relaxation
- Stroke Volume (SV) = Blood volume ejected per contraction (~80 mL)
- Heart Rate (HR) = Beats per minute
- Cardiac Output (CO) = Volume of blood pumped per minute
- CO = HR × SV
- Chronotropic influences = Modify HR
- Inotropic influences = Modify contractility (and SV)
- Dromotropic influences = Modify AV node conduction delay
- End Diastolic Volume (EDV) = Volume at end of ventricular filling (~130 mL)
- End Systolic Volume (ESV) = Volume after systole (~50 mL)
- Preload = Ventricular stretch during diastole
- ↑ Preload → ↑ myofibril stretch → ↑ force of contraction (Frank–Starling mechanism)
- Afterload = Pressure the ventricle must overcome to eject blood
- ↑ Afterload → ↓ stroke volume due to reduced ejection time
Overview of the Cardiac Cycle (Diagram)
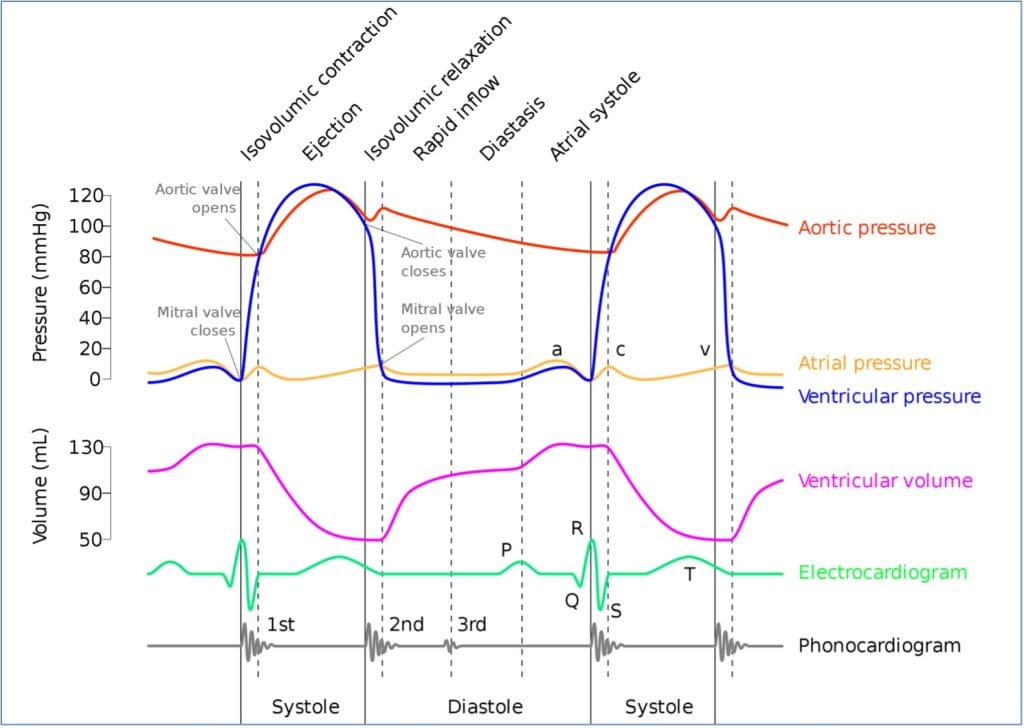
Phases of the Cardiac Cycle
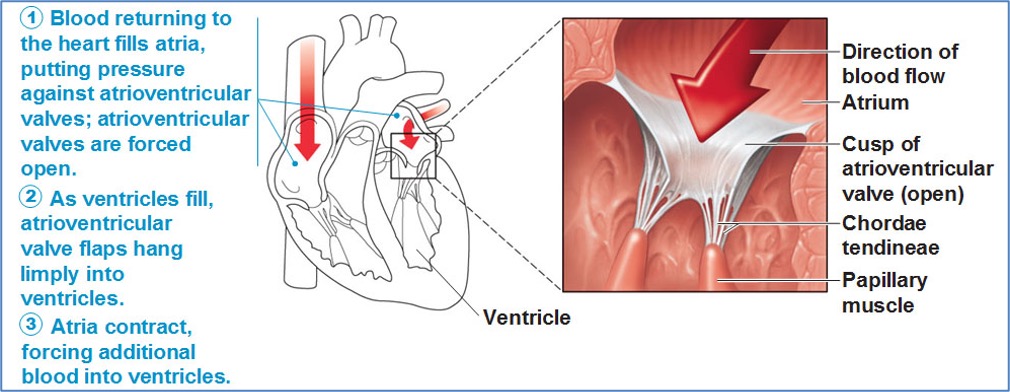
Phase 1 – Atrial Contraction (Atrial Systole)
- Atria contract → ↑ atrial pressure
- Blood pushed into ventricles through AV valves
- Ventricles are already ~70% full from passive venous filling
- End result: Ventricles reach EDV ≈ 130 mL
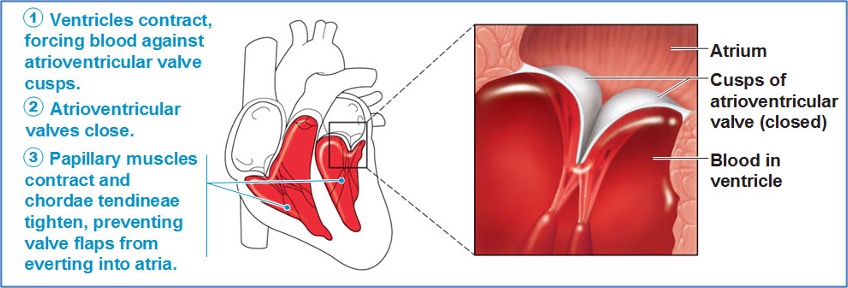
Phase 2 – Ventricular Systole
a) AV Valves Close (Isovolumetric Contraction)
- Ventricular pressure exceeds atrial pressure → AV valves shut
- All valves are closed
- Pressure rises without volume change
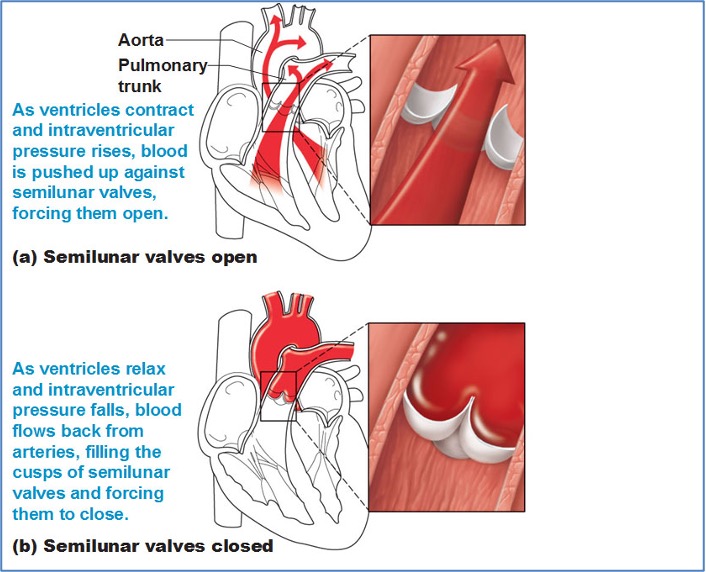
b) Semilunar Valves Open (Ejection Phase)
- Ventricular pressure exceeds aortic/pulmonary pressure
- SL valves open → ~80 mL ejected per ventricle (stroke volume)
- Ventricular volume decreases
c) Semilunar Valves Close
- Ventricular pressure drops below aortic/pulmonary artery pressure
- SL valves close, producing dicrotic notch
- Brief rise in aortic pressure due to blood rebound and vessel elasticity
- ~50 mL remains in ventricle = ESV
Phase 3 – Ventricular Diastole
- Ventricular pressure drops below atrial pressure
- AV valves open
- Blood flows passively from atria into ventricles
- Passive filling accounts for ~70% of ventricular volume

Summary – Cardiac Cycle Physiology
Cardiac cycle physiology explains the sequence of systole and diastole that drives blood through the heart. Coordinated contraction and relaxation phases ensure optimal preload, ejection, and filling. Stroke volume and cardiac output depend on preload, afterload, and inotropic/chronotropic control. For a broader context, see our Cardiovascular Overview page.