Table of Contents
Overview – Electrophysiology of the Heart
Electrophysiology of the heart refers to the electrical conduction system that drives each heartbeat. Unlike skeletal muscle, the heart contracts without direct neural input from the brain. Instead, it uses a specialised network of pacemaker and contractile cells to generate and propagate action potentials, ensuring coordinated contraction of the atria and ventricles. This topic is vital for understanding arrhythmias, ECG interpretation, and pharmacologic targets in cardiovascular care.
The Heartbeat and Its Autonomy
- The heart is a muscle that requires:
- Oxygen
- Nutrients
- Action potentials to function
- Unlike skeletal muscle, it does not require brain input
- Heart has its own conduction system
- Can beat autonomously, which explains why transplanted hearts continue to beat with adequate O₂ and nutrients
- Effective cardiac function requires coordinated contraction of atria and ventricles
- This is achieved through the heart’s intrinsic electrical conduction system
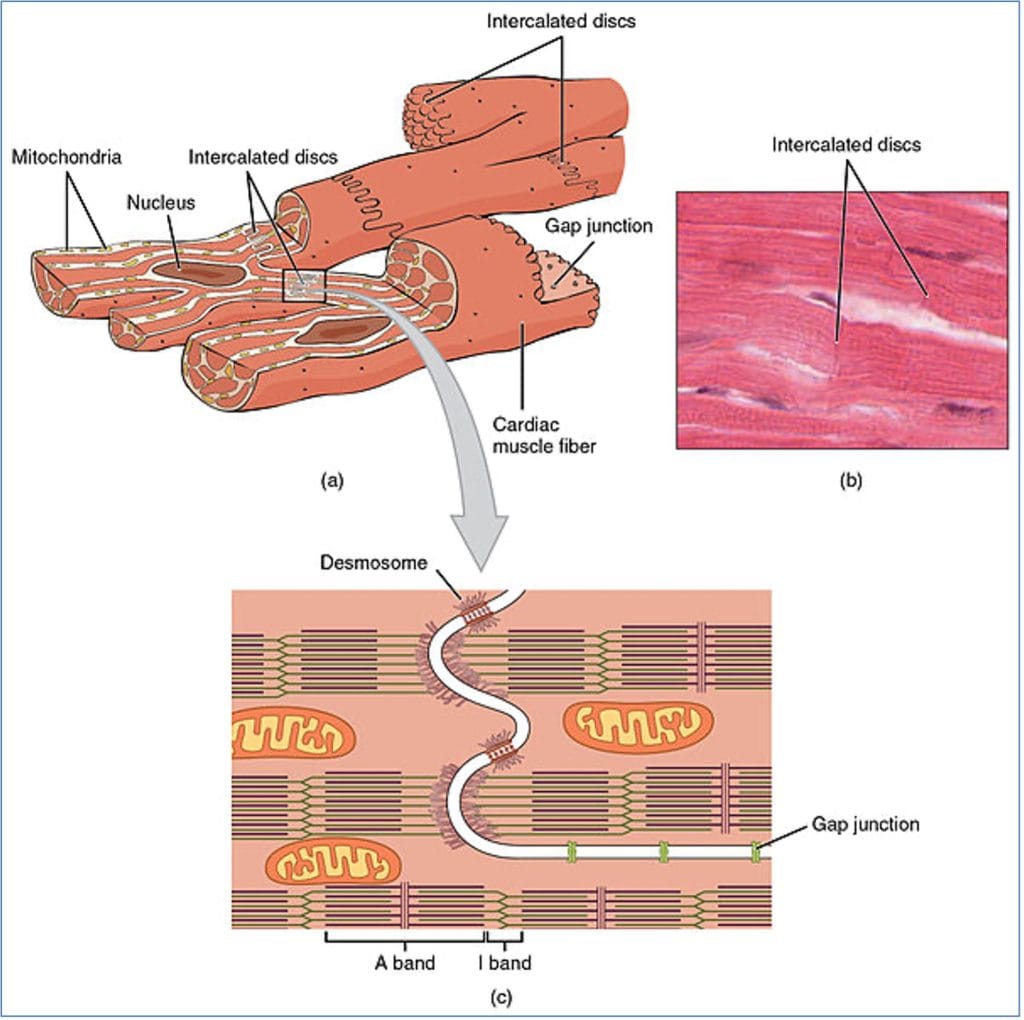
Electrical Connectivity of the Heart
- The entire myocardium is electrically connected via:
- Gap junctions: Allow direct passage of ions and action potentials between cells
- Intercalated discs: Mechanically and electrically connect cardiac cells, supporting synchronised contraction
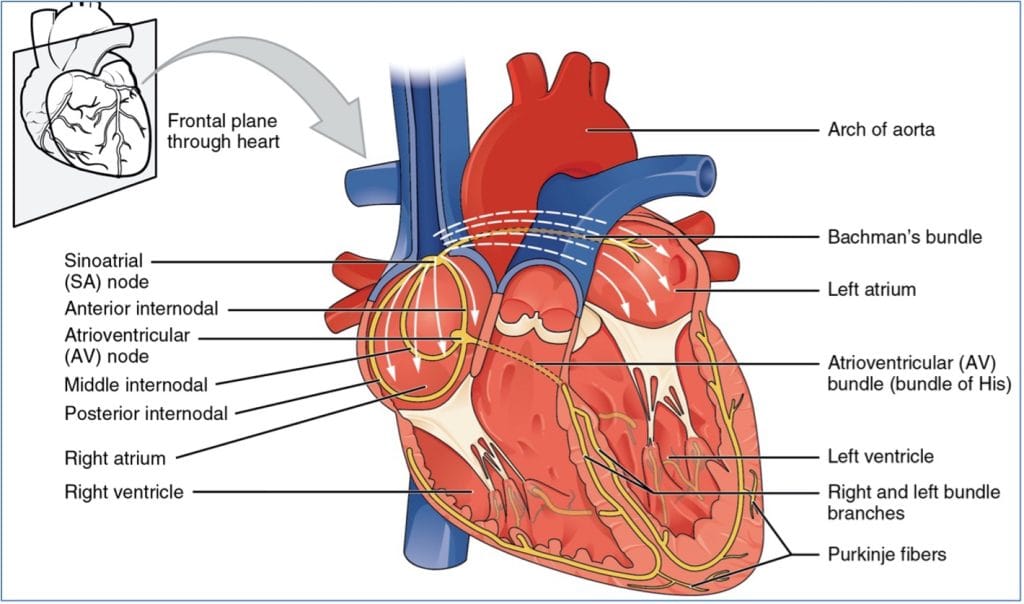
The Cardiac Conduction System
Order of signal transmission:
Sinoatrial (SA) Node → Atrioventricular (AV) Node → Bundle of His → Right & Left Bundle Branches → Purkinje Fibres → Myocyte Contraction
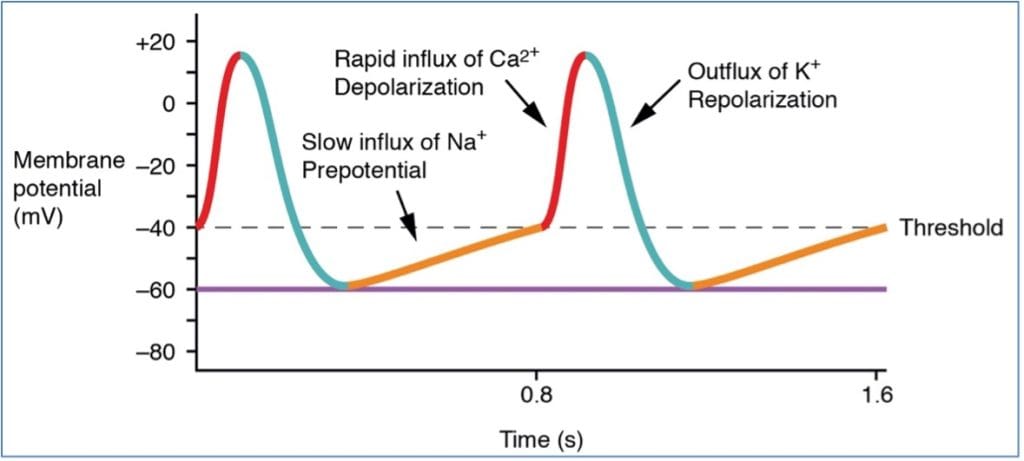
Conductile Cardiac Cell Physiology (SA/AV Node Cells)
- Pacemaker cells exhibit slow-type action potentials
- Unstable resting membrane potential leads to spontaneous depolarisation (Prepotential phase)
- Caused by leaky Na⁺ channels
- Depolarisation phase:
- Once threshold reached → Ca²⁺ channels open → Influx of Ca²⁺ → Action potential
- Repolarisation phase:
- Ca²⁺ channels close
- K⁺ channels open → Efflux of K⁺ → Membrane repolarises
- Note:
- Na⁺ initiates prepotential, but Ca²⁺ is responsible for depolarisation
- Control Hierarchy:
- SA Node has the highest intrinsic rate and normally dominates pacing
Contractile Cardiac Cell Physiology (Purkinje Fibres & Myocytes)
- Exhibit fast-type action potentials
- Have stable resting membrane potential
Phases of Action Potential:
- Resting Phase
- Na⁺ and Ca²⁺ channels are closed
- Depolarisation
- Membrane potential rises → Fast Na⁺ channels open → Rapid Na⁺ influx
- Plateau Phase
- Na⁺ channels inactivate
- Small initial drop from K⁺ efflux
- Voltage-gated Ca²⁺ channels open → Ca²⁺ influx
- Triggers Ca²⁺-induced Ca²⁺ release from sarcoplasmic reticulum
- Leads to contraction
- Plateau is maintained by balanced Ca²⁺ influx and K⁺ efflux
- Repolarisation
- Ca²⁺ channels close
- K⁺ channels stay open → Net outward current → Membrane returns to resting
- More K⁺ channels open as repolarisation proceeds
- Final steps: majority of K⁺ channels close
Ion Restoration:
- Na⁺/K⁺-ATPase:
- Removes excess intracellular Na⁺
- Replaces lost intracellular K⁺
- Na⁺/Ca²⁺ Exchanger:
- Eliminates excess intracellular Ca²⁺
NOTE: There is a considerable delay between Myocardial Contraction & the Action Potential.
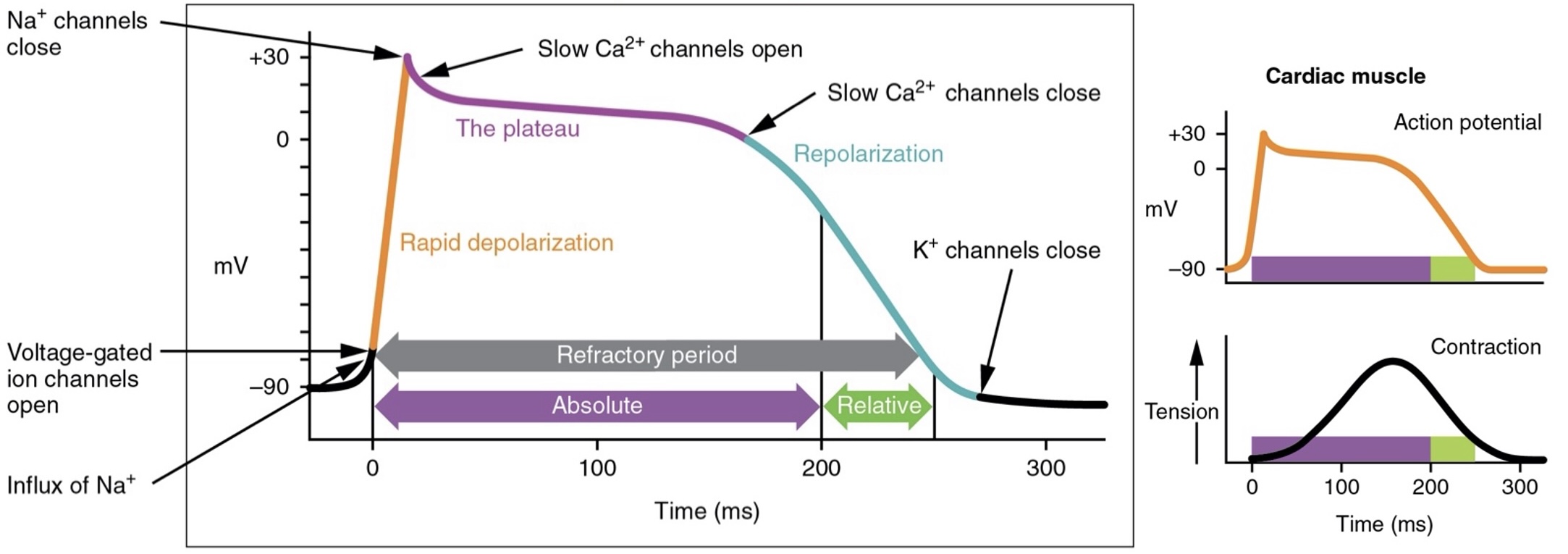
Refractory Periods
- Cardiac muscle exhibits prolonged refractory periods
- Prevents tetany (sustained contraction) — essential for rhythmic pumping
- Absolute Refractory Period:
- ~200 ms
- Duration: from peak depolarisation → plateau → halfway through repolarisation
- No second action potential can occur during this phase
- Relative Refractory Period:
- ~50 ms
- Na⁺ channels are closed but excitable with a strong stimulus
- Occurs during latter half of repolarisation
Sinoatrial (SA) Node
- Primary pacemaker of the heart
- Intrinsic rate: 90–100 bpm (unmodulated)
- Parasympathetic nervous system:
- Lowers heart rate to ~70 bpm at rest
- Sympathetic nervous system:
- Increases heart rate during stress or exertion
Location
- Posterior wall of the right atrium
- Near the opening of the superior vena cava
Action Potentials
- Continuously depolarises at its intrinsic rate
- Action potential takes ~50 ms to reach the AV node
Role in Conduction
- Sets the pace for the entire heart
- Initiates contraction of the right and left atria
Atrioventricular (AV) Node
- Second in command
- Intrinsic rate: 40–60 bpm
Location
- Inferior interatrial septum, just above the tricuspid valve
Action Potentials
- Spontaneous depolarisation at a slower rate than SA node
Role in Conduction
- Delays the impulse from SA node by ~100 ms
- Allows full atrial contraction before ventricular contraction
- Conducts impulse to Bundle of His → Purkinje fibres
Area Served
- Transmits signal from atria to ventricles via the conduction network
Bundle of His (Atrioventricular Bundle)
- Third in command
- Intrinsic rate: 20–40 bpm
Location
- Begins at the superior interventricular septum
Action Potentials
- Slower than SA and AV nodes
- Capable of autonomous depolarisation
Role in Conduction
- Only electrical connection between atria and ventricles
- Transmits impulse from AV node to left and right bundle branches
Area Served
- Conducts signals down the septum toward the apex of the heart
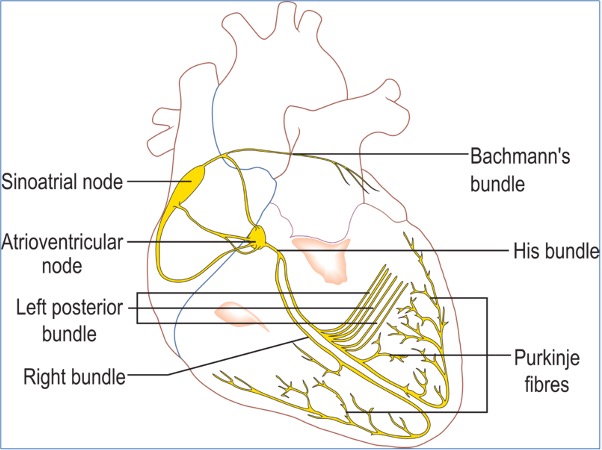
Purkinje Fibres
- Specialised conducting myocytes
- Contain few myofibrils, so do not contract during impulse transmission
- Intrinsic rate: ~15 bpm (least dominant pacemaker)
Location
- Subendocardial layer of ventricular walls
- Originate at the apex and spread superiorly within the ventricular myocardium
Action Potentials
- Fast depolarisation
- Long plateau and refractory period
- Conductile, but resemble those of ventricular muscle fibres
Role in Conduction
- Deliver impulses to ventricular myocardium
- Trigger synchronous ventricular contraction

Autonomic Nervous System Effects
The heart is autonomously active but modulated by ANS input to regulate rate and force based on systemic demands.
Parasympathetic Nervous System
- Innervates SA and AV nodes
- Neurotransmitter: Acetylcholine
- Binds to muscarinic receptors →
- Increases K⁺ efflux → hyperpolarisation
- Slower drift to threshold → reduced firing rate
- → Decreases heart rate
Sympathetic Nervous System
- Innervates SA node, AV node, and ventricular muscle
- Neurotransmitter: Noradrenaline (norepinephrine)
- Binds to β₁-adrenergic receptors →
- Activates cyclic AMP pathway
- → Increases Na⁺ and Ca²⁺ permeability in nodal tissue
- → Accelerates depolarisation → increased heart rate
On Contractile Tissue:
- Increases Ca²⁺ influx through membrane
- Enhances Ca²⁺ release from sarcoplasmic reticulum (SR)
- → Boosts contractile force of myocardium

Summary – Electrophysiology of the Heart
Electrophysiology of the heart involves the generation and propagation of action potentials that coordinate cardiac contraction without central nervous system input. Pacemaker cells initiate the electrical rhythm, while contractile cells propagate and respond to it, ensuring efficient cardiac output. These principles underpin ECG interpretation and treatment of arrhythmias. For a broader context, see our Cardiovascular Overview page.