Table of Contents
Overview
Heart failure is a clinical syndrome in which the heart is unable to pump sufficient blood to meet the metabolic demands of the body, resulting in inadequate organ perfusion and fluid accumulation. Heart failure remains a major global burden, with significant morbidity and a 30% mortality rate within the first year of diagnosis. Understanding the pathophysiology, classification, and management of heart failure is essential for final-year medical students preparing for clinical practice.
Definition
Heart failure is defined as the inability of the heart to provide adequate cardiac output to meet the body’s metabolic needs, either due to impaired systolic contraction, diastolic filling, or both.
Aetiology
Myocardial Causes
- Ischaemic heart disease
- Cardiomyopathies (e.g. dilated, hypertrophic)
- Myocarditis
- Alcohol-related myocardial dysfunction
Valvular Causes
- Aortic or mitral stenosis
- Regurgitation of aortic or mitral valves
Circulatory/Systemic Causes
- Severe anaemia
- Thyrotoxicosis
- Shock or haemorrhage
Pathophysiology
- Systolic dysfunction: Impaired contraction → reduced ejection fraction
- Diastolic dysfunction: Stiff ventricular walls → impaired filling
- Forward failure: ↓ Cardiac output → ↓ organ perfusion
- Backward failure: Venous congestion behind failing ventricle
Compensatory Mechanisms
- Frank-Starling mechanism: ↑ Preload → ↑ Stroke volume (short-term benefit, long-term harm)

- Myocardial hypertrophy:
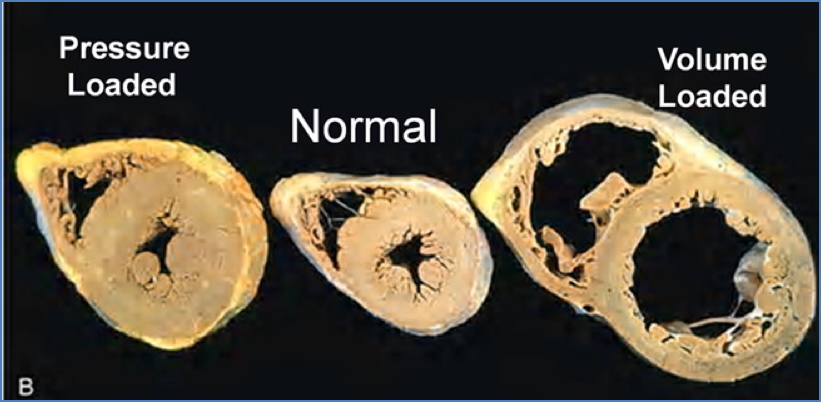
- Concentric hypertrophy = Pressure overload → ↓ compliance
- Eccentric hypertrophy = Volume overload → dilation, weak contraction
- Neurohormonal responses:
- ↑ Noradrenaline/Adrenaline → ↑ HR, contractility, vasoconstriction
- RAAS activation → Fluid retention, ↑ preload and afterload
- Atrial Natriuretic Peptide (ANP) release → Vasodilation, natriuresis (compensatory)

Clinical Features
Symptoms
- Dyspnoea (exertional, orthopnoea, paroxysmal nocturnal)
- Fatigue and reduced exercise tolerance
- Cough with frothy sputum
- Peripheral oedema
Signs
- Low BP, thready pulse
- Tachycardia (compensatory)
- Raised JVP
- Basal crackles
- Hepatomegaly, ascites, pleural effusions
NYHA Classification
- Class I: No symptoms
- Class II: Symptoms on moderate exertion
- Class III: Symptoms on mild exertion
- Class IV: Symptoms at rest
- Class V: Bedbound, life support dependent
Left vs Right Heart Failure
Left-Sided
- ↓ LV output to systemic circulation
- Common causes: IHD, cardiomyopathies, hypertension, aortic stenosis
- Symptoms: Pulmonary congestion → cough, orthopnoea, PND
- Complications: Renal dysfunction, altered mental status
Right-Sided
- ↓ RV output to pulmonary circulation
- Common cause: Left-sided heart failure (Cor pulmonale)
- Symptoms: Peripheral oedema, ascites, hepatomegaly

Investigations
- BNP >500 pg/mL: Suggestive of heart failure
- Chest X-ray: Cardiomegaly, pulmonary oedema, effusions
- ECG: Ischaemia, arrhythmias
- Echocardiogram (TTE/TOE): Assess EF, wall motion, valve function
- Bloods:
- FBC (anaemia, infection)
- UEC (renal function)
- LFTs (alcohol-related disease)
- TSH (thyroid function)
- Lipids, BSL, HbA1c (comorbidities)
Management
Chronic Heart Failure
- Address Comorbidities: COPD, diabetes, infection, thyroid disease
- Lifestyle Modifications: Reduce alcohol, smoking, salt; weight loss
- Pharmacological Therapy:
- ACEi (Perindopril) or ARB (Candesartan): ↓ preload and afterload
- β-blockers (Carvedilol, Metoprolol, Bisoprolol): ↓ HR and cardiac workload
- Loop diuretics (Frusemide): Symptomatic relief of fluid overload
- Spironolactone: In severe cases; also K+ sparing
- Digoxin (optional): Symptom relief, especially in AF
- Vasodilators (Hydralazine, nitrates): Adjunctive
- Oxygen therapy: If SpO₂ < 88%
- ICD: In high-risk patients to prevent sudden arrhythmic death
Acute Decompensated Heart Failure
- Intensify chronic therapy: ↑ Frusemide
- Add Digoxin for inotropic support
- Consider intravenous nitrates
Complications
- Sudden cardiac death due to ventricular tachycardia/fibrillation
- Cardiogenic pulmonary oedema
- Thromboembolism (from mural thrombus)
- Multi-organ dysfunction (renal, hepatic, cerebral)
Summary
Heart failure is a complex clinical syndrome resulting from inadequate cardiac output to meet the body’s demands. It can be caused by myocardial, valvular, or circulatory pathology and typically presents with fatigue, dyspnoea, and signs of fluid overload. The condition is classically divided into left- and right-sided heart failure, each with distinct but often overlapping features. Management involves treating the underlying cause, optimising pharmacological therapy, and implementing lifestyle changes. For more information, visit our Cardiovascular Overview page.