Table of Contents
Overview – Pericarditis
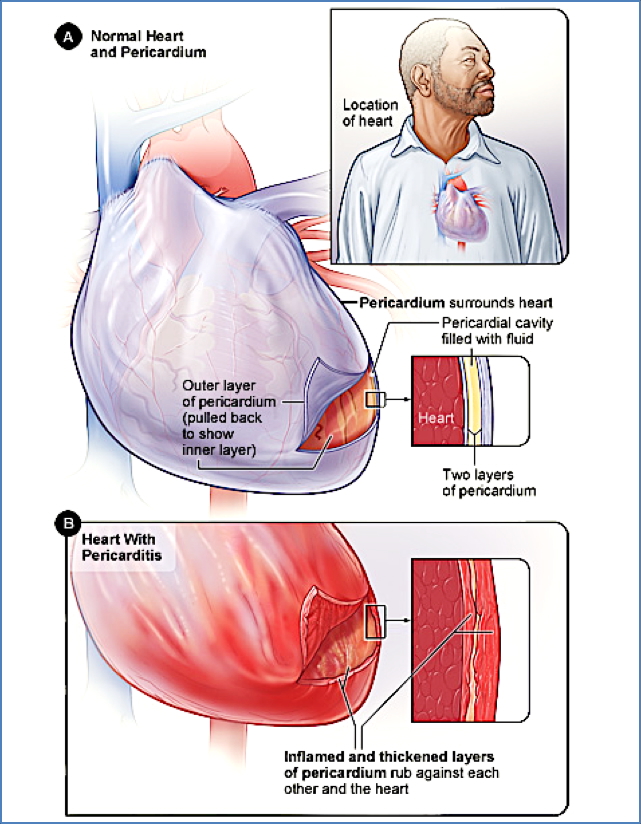
Pericarditis is inflammation of the pericardium, the fibrous sac surrounding the heart. It commonly presents with pleuritic chest pain and can result from infections, autoimmune conditions, or post-injury inflammation. Pericarditis may lead to complications such as pericardial effusion, cardiac tamponade, or—if chronic—constrictive pericarditis. Prompt diagnosis and management are crucial to prevent life-threatening sequelae.
Definition
Pericarditis refers to acute or chronic inflammation of the pericardial sac, often with accumulation of pericardial exudate and potential compromise of cardiac function.
Aetiology
- Infectious causes:
- Viruses (most common)
- Bacteria (e.g. TB)
- Fungi, parasites
- Immune-mediated:
- Rheumatic fever
- Systemic lupus erythematosus (SLE)
- Post-myocardial infarction (Dressler syndrome)
- Drug hypersensitivity
- Other causes:
- Post-cardiac surgery
- Malignancy
- Trauma
- Radiation
Classification (by Exudate Type)
- Serous – Seen in SLE, uraemia, tumours
- Purulent – Bacterial infections
- Fibrinous/Serofibrinous – Post-MI, SLE, trauma, radiation
- Caseous – Tuberculosis
- Haemorrhagic – Seen with malignancy or after cardiac surgery
Pathogenesis
Various triggers induce pericardial inflammation → thickening of pericardium and formation of exudate (serous fluid ± pus/fibrin/blood) → rubbing of inflamed layers → further inflammation and fluid accumulation.
Clinical Features
Symptoms
- Sharp, pleuritic chest pain (improves when sitting forward, worse on inspiration/lying down)
- Fever
- Fatigue
- Dry cough
- Dyspnoea (especially if effusion is present)
Signs
- Tachycardia
- Pericardial friction rub
- Muffled heart sounds
- Elevated JVP
- Signs of tamponade or heart failure in severe cases
Complications
- Cardiac tamponade
- Pericardial effusion
- Chronic pericarditis → Constrictive pericarditis (>3 months)
Investigations
- ECG – PR depression, widespread ST elevation, tachycardia
- CXR – May show cardiomegaly or pulmonary congestion
- Echocardiogram – To assess for pericardial effusion
- Consider ESR, CRP, troponins to assess inflammation and cardiac injury
Management
- Treat the underlying cause
- NSAIDs or corticosteroids for inflammation
- Analgesia for pain control
- Monitor for complications such as effusion or tamponade
Constrictive Pericarditis
Definition
A chronic form of pericarditis where the pericardium becomes fibrotic, thickened, adherent, and/or calcified, restricting diastolic filling.
Aetiology
- Chronic progression from acute pericarditis
- Tuberculosis, post-radiation, post-cardiac surgery, idiopathic
Symptoms
- Dyspnoea
- Fatigue
- Palpitations
- Abdominal pain
Signs
- Features mimicking right-sided heart failure:
- Ascites
- Hepatosplenomegaly
- Peripheral oedema
- Elevated JVP
- Kussmaul’s sign: JVP rises with inspiration
- Friedrich’s sign: prominent Y-descent in JVP
- Pericardial knock: early diastolic sound
- BP normal or low ± pulsus paradoxus
Investigations
- ECG – Low voltage QRS, flat T-waves, ± atrial fibrillation
- CXR – May show calcification or effusion
- CT/MRI/TEE – Pericardial thickening
- Cardiac catheterisation – Equalised diastolic pressures in all chambers, RVEDP >1/3 systolic pressure
Management
- Medical:
- Diuretics
- Salt restriction
- Surgical:
- Pericardiectomy for definitive relief
Summary – Pericarditis
Pericarditis is inflammation of the pericardial sac often caused by infections, autoimmune diseases, or trauma. It typically presents with pleuritic chest pain and may progress to pericardial effusion or tamponade. Chronic inflammation can lead to constrictive pericarditis, which mimics right heart failure and may require pericardiectomy. For a broader context, see our Cardiovascular Overview page.