Table of Contents
Overview – Chronic Skin Ulcers
Chronic skin ulcers refer to persistent skin breakdown, most commonly affecting the lower limbs, that fails to heal over time due to underlying vascular, neuropathic, or pressure-related causes. Chronic skin ulcers are clinically significant due to their prolonged course, risk of infection, and association with systemic disease, particularly diabetes and peripheral vascular disease. Accurate classification into venous, arterial, neuropathic, or pressure ulcers is key for targeted management and prevention of complications.
Definition
Chronic skin ulcers are defined as skin lesions that fail to heal within six weeks, usually secondary to impaired perfusion, mechanical pressure, or loss of protective sensation.
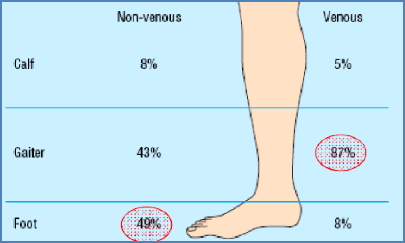
Most Common Locations
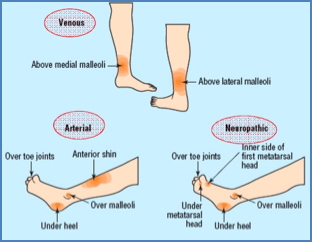
- Venous –“Gaiter” Region
- Arterial – Foot Region, Anterior Shin & Pressure Points
- Neuropathic –Pressure Points
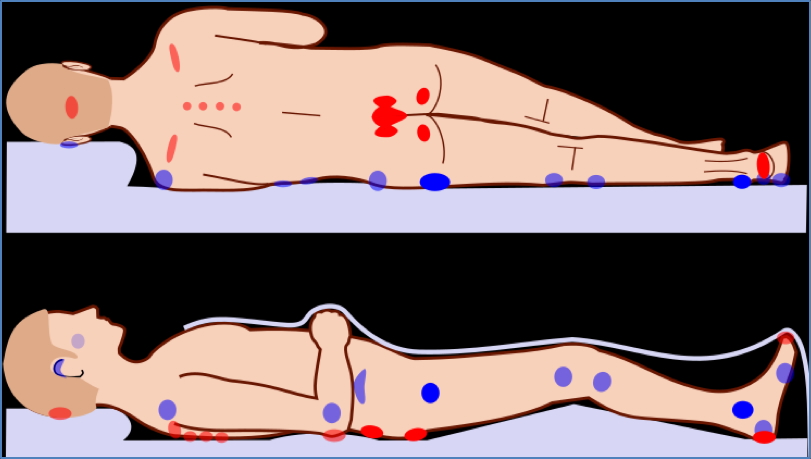
Pressure Ulcers
- Aetiology:
- Sustained pressure in immobile or frail patients (e.g. bedridden, paraplegia)
- Pathogenesis:
- Prolonged pressure → tissue ischaemia and necrosis
- Location:
- Bony prominences (sacrum, heels, elbows, occiput)
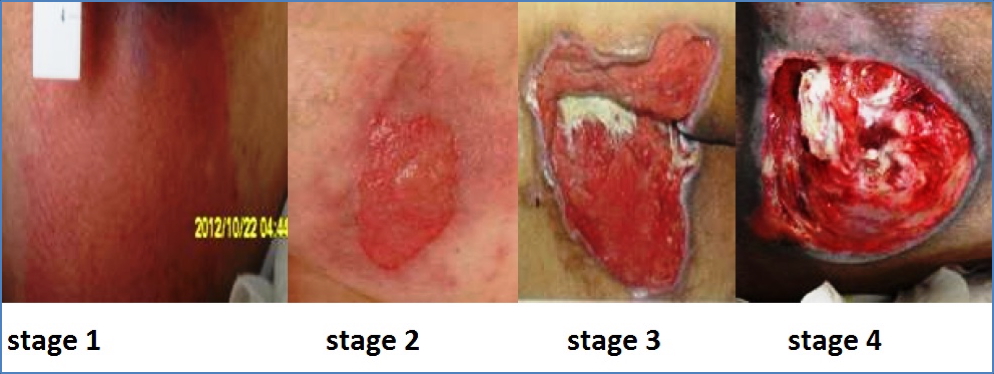
- Appearance:
- Initially presents as non-blanching erythema
- Progresses to ulceration with wet, oozing base
- Symptoms:
- Painful unless sensory neuropathy present
- Management:
- Pressure relief (regular turning, specialised mattress)
- Wound debridement and dressings
- Antibiotics if infected
Arterial Ulcers
- Aetiology:
- Peripheral arterial disease (PVD), most commonly due to atherosclerosis
- Common in diabetics
- Pathogenesis:
- Arterial insufficiency → tissue hypoxia → ulceration following minor trauma
- Location:
- Anterior shin, pressure points of the foot (e.g. heel, toes)
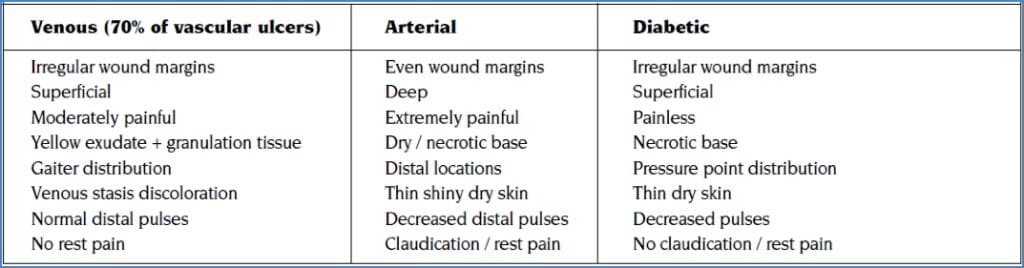
- Appearance:
- Well-defined, pale, dry base, often necrotic
- Does not bleed easily
- Cold, pulseless extremity
- Symptoms:
- Severe pain, relieved by leg dependency
- Claudication
- Management:
- DO NOT use compression
- Risk factor control (smoking, diabetes, hypertension, dyslipidaemia)
- Revascularisation (angioplasty or surgical bypass)
- Debridement as needed


Venous Ulcers
- Aetiology:
- Chronic venous insufficiency due to valve incompetence → venous hypertension
- Often associated with varicose veins
- Pathogenesis:
- Venous stasis → oedema → skin breakdown
- Location:
- Gaiter region (above the medial malleolus)
- Appearance:
- Irregular margins
- Moist, granulating base
- Surrounding stasis dermatitis and oedema
- Bleeds on touch
- Symptoms:
- Mild pain, worse with dependency and improved by elevation
- Management:
- Compression bandages
- Leg elevation and exercise
- Wound cleaning and dressings


Neuropathic (Diabetic) Ulcers
- Aetiology:
- Diabetic peripheral neuropathy ± arterial insufficiency
- Pathogenesis:
- Loss of sensation → unnoticed trauma at pressure points → ulceration
- Location:
- Pressure areas (e.g. heel, metatarsal heads)
- Appearance:
- Punched-out, deep ulcers
- Surrounded by callus (hyperkeratosis)
- Dry, non-bleeding base
- Symptoms:
- Typically painless
- Management:
- DO NOT apply compression
- Meticulous foot care (podiatrist input essential)
- Debridement ± amputation
- Antibiotics for infection
- Strict diabetes and cardiovascular risk factor control

Differential Diagnosis
- Pyoderma gangrenosum
- Malignant ulcers (e.g. Marjolin’s ulcer)
- Vasculitic ulcers
- Traumatic wounds
- Fungal or mycobacterial infections
Summary – Chronic Skin Ulcers
Chronic skin ulcers encompass a range of persistent wounds including venous, arterial, neuropathic, and pressure ulcers, each with distinct pathogenesis, appearance, and management. Accurate diagnosis and tailored treatment are essential for healing and prevention of recurrence. For a broader context, see our Cardiovascular Overview page.