Table of Contents
Overview – Dyslipidaemia
Dyslipidaemia is a broad term referring to elevated levels of cholesterol, triglycerides, or both in the bloodstream. It is a major modifiable risk factor for atherosclerosis, cardiovascular disease (CVD), and stroke. Dyslipidaemia may be primary (genetic) or secondary (acquired), and its detection and management are essential in both prevention and treatment of heart disease.
Lipid Physiology
Lipid Transporters
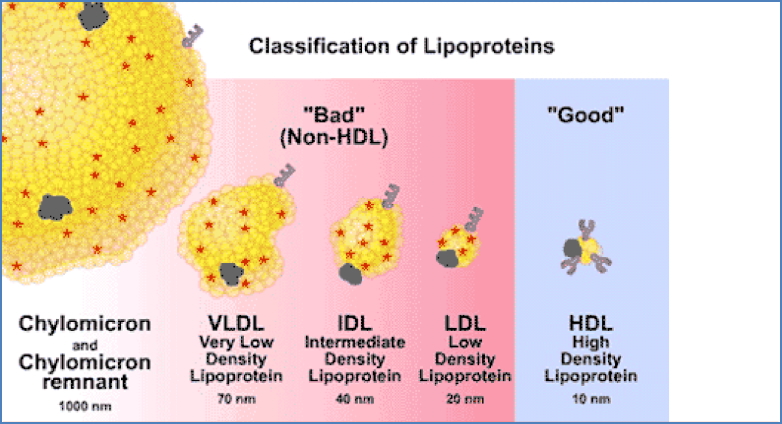
- Chylomicrons – Synthesised by the small intestine; transport dietary fats to the liver via the lymphatic system.
- Very Low Density Lipoproteins (VLDL) – Produced by the liver; transport triglycerides and cholesterol to peripheral tissues.
- Intermediate Density Lipoproteins (IDL) – Derived from VLDLs after removal of some lipid and protein.
- Low Density Lipoproteins (LDL) – “Bad” cholesterol; delivers cholesterol to tissues and contributes to atherosclerosis when elevated.
- High Density Lipoproteins (HDL) – “Good” cholesterol; mediates reverse cholesterol transport from tissues back to the liver.
Aetiology
Primary (Genetic) Causes
- Familial hyperlipidaemia
- Lipoprotein lipase deficiency
Secondary (Acquired) Causes
- Obesity
- Hypothyroidism
- Diabetes mellitus
- Nephrotic syndrome
- Liver failure
- Medications (e.g. oral contraceptives, retinoids, thiazide diuretics)
Diagnosis & Screening
Screen individuals with:
- Family history of CVD, ischaemic heart disease (IHD), myocardial infarction (MI), or hypercholesterolaemia
- Clinical signs (e.g. xanthomata, xanthelasma)
- Relevant comorbidities (e.g. obesity, diabetes, hypertension, hypothyroidism)
Investigations
- Triglycerides (TGLs)
- Normal: <2 mmol/L
- Intervention threshold: >6 mmol/L
- Lifestyle changes for 6 months → Statin therapy if no improvement
- Total Cholesterol
- Normal: <4 mmol/L
- Intervention threshold: >6.5 mmol/L
- Lifestyle changes for 6 months → Statin therapy
- Target: <4 mmol/L total cholesterol or LDL-C <1.8 mmol/L
Management
1. Lifestyle Modification
- Diet: ↓ Saturated fat and cholesterol; ↑ fibre; reduce alcohol and smoking; weight loss
- Exercise: Regular physical activity
2. Pharmacological Therapy
Statins (HMG-CoA Reductase Inhibitors)
- Examples: Simvastatin, Atorvastatin
- Mechanism: Inhibit HMG-CoA reductase → ↓ hepatic cholesterol synthesis
- Side Effects:
- Statin-induced myopathy/myositis/rhabdomyolysis
- Monitor for muscle pain/weakness and ↑ creatine kinase (CK)
Other Lipid-Lowering Agents (use if CHD or statin-intolerant)
- Fibrates (e.g. fenofibrate)
- Bile acid-binding resins (e.g. cholestyramine)
- Ezetimibe – inhibits intestinal cholesterol absorption
- Fish oil (Omega-3 fatty acids) – possible prophylactic use
Summary – Dyslipidaemia
Dyslipidaemia refers to abnormal lipid profiles, including elevated LDL or triglycerides, or reduced HDL levels. Early detection via lipid screening, lifestyle interventions, and pharmacologic therapy — particularly with statins — are critical in preventing atherosclerosis and cardiovascular disease. For broader clinical context, see our Cardiovascular Overview page.