Table of Contents
Overview – Hypertension
Hypertension is a persistently elevated arterial blood pressure that significantly increases the risk of stroke, myocardial infarction, heart failure, chronic kidney disease, and peripheral vascular disease. It is often asymptomatic but is a major modifiable risk factor for cardiovascular and end-organ complications. This article outlines the definitions, causes, diagnostic workup, and management of hypertension, tailored to final-year medical students preparing for clinical application.
Definition
- Hypertension (HTN):
- Systolic BP ≥ 140 mmHg and/or
- Diastolic BP ≥ 90 mmHg
- Requires 3 separate readings over 6 months for formal diagnosis
- Stage-based classification (Adults):
| Category | Systolic (mmHg) | Diastolic (mmHg) | % of Population |
|---|---|---|---|
| Normal | 120–140 | 80–90 | 83% |
| Stage 1 Hypertension (Mild) | 140–160 | 90–100 | 13.5% |
| Stage 2 Hypertension (Moderate) | 160–180 | 100–110 | 2% |
| Stage 3 Hypertension (Severe) | 180–210 | 110–120 | 1% |
| Stage 4 Hypertension (Severe) | ≥210 | ≥120 | 0.5% |
Aetiology
Primary (Essential) Hypertension – 95%
- Idiopathic and multifactorial
- Common risk factors:
- Family history, high salt/cholesterol intake
- Obesity, diabetes mellitus, smoking
- Excess alcohol, stress, increasing age
- Subtypes:
- Isolated Diastolic Hypertension: Often older males
- Isolated Systolic Hypertension:
- Young adults → ↑ Cardiac output (sympathetic overactivity)
- Elderly → ↓ Arterial compliance (vascular stiffening)
Secondary Hypertension – 5%
- Cardiac causes: Coarctation of aorta, hypervolaemia
- Renal causes: CKD, glomerulonephritis, renal artery stenosis
- Endocrine causes: Cushing’s, acromegaly, pheochromocytoma, thyroid dysfunction
- Neurologic causes: Raised intracranial pressure, sleep apnoea, acute stress
- Pregnancy-related: Pre-eclampsia – placental ischaemia leads to vasoconstrictive mediators
Pathophysiology
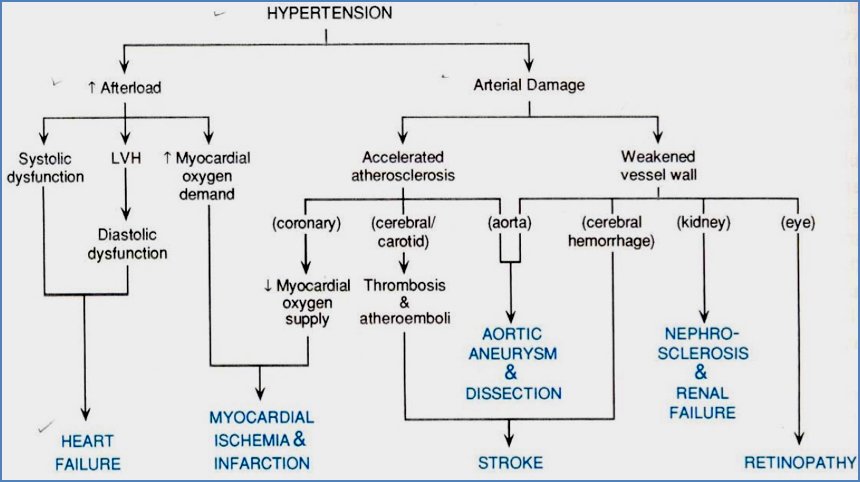
- Hypertension increases afterload, requiring the heart to work harder
- Chronic elevation → left ventricular hypertrophy, impaired relaxation, reduced cardiac output
- Accelerated vascular damage → arteriosclerosis, microangiopathy, and end-organ damage
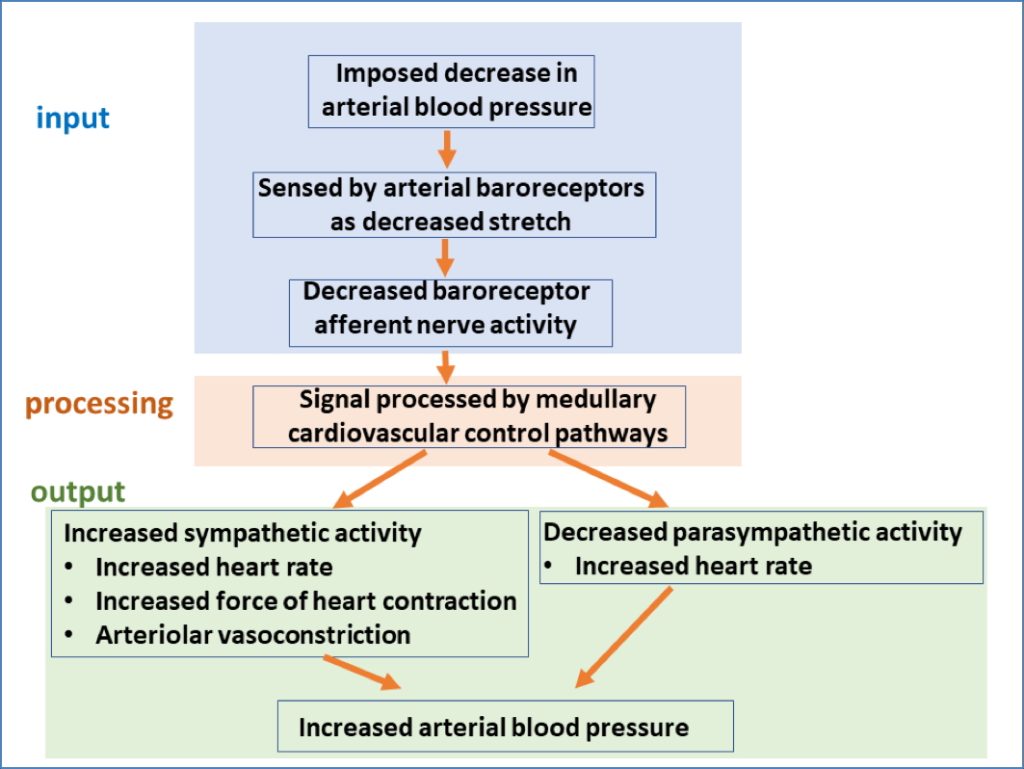
- Baroreceptor reflex: Acts to correct acute BP drops but is reset in chronic HTN
Clinical Features
- Symptoms: Often asymptomatic
- If severe: Headache, dizziness, visual disturbance, nausea, vomiting
- Signs:
- Features of underlying cause: goitre (thyroid), abdominal masses (adrenal or renal), signs of CKD
- Fundoscopy: hypertensive retinopathy (e.g., papilloedema)
- Cardiovascular: displaced apex beat, murmurs
- Renal bruit in renal artery stenosis
Investigations
- Diagnosis:
- 3 elevated readings over 6 months
- Confirm with home or ambulatory monitoring, especially in “white coat” HTN
- Standing BP:
- Diastolic ↑ on standing → Essential HTN
- Diastolic ↓ on standing → Secondary HTN
- Workup:
- FBC – rule out polycythaemia
- UEC – assess renal function, electrolyte status
- Lipid profile – assess cardiovascular risk
- Urinalysis – proteinuria or haematuria (renal disease)
- BSL – diabetes screening
- ECG – evidence of LVH or ischaemia
Management
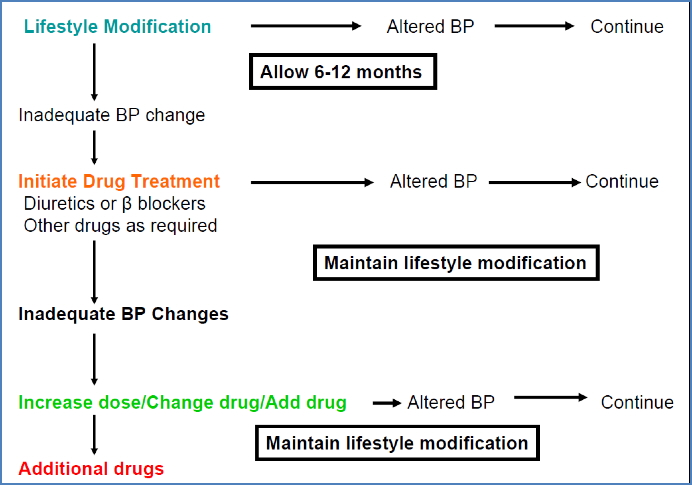
Lifestyle Changes
- Weight loss
- Smoking cessation
- Salt/alcohol reduction
- Low-fat diet
- Regular aerobic exercise
Pharmacological Management
- Initiate if BP >160/100 mmHg (Stage 2)
- Stepwise approach:
- Monotherapy, then combine if needed
- ACE inhibitors (Perindopril) or ARBs (Candesartan)
- Calcium channel blockers (Amlodipine, Nifedipine)
- Thiazide diuretics (Hydrochlorothiazide)
- Beta-blockers (Carvedilol, Atenolol) – only if IHD or heart failure
- Therapeutic target:
- <140/90 mmHg general population
- <130/80 mmHg in diabetics
- Monotherapy, then combine if needed
- Mechanisms of Action:
- Diuretics: Reduce blood volume → ↓ Preload
- Sympatholytics: ↓ HR and contractility → ↓ Cardiac output
- Vasodilators: ↓ Peripheral resistance → ↓ Afterload
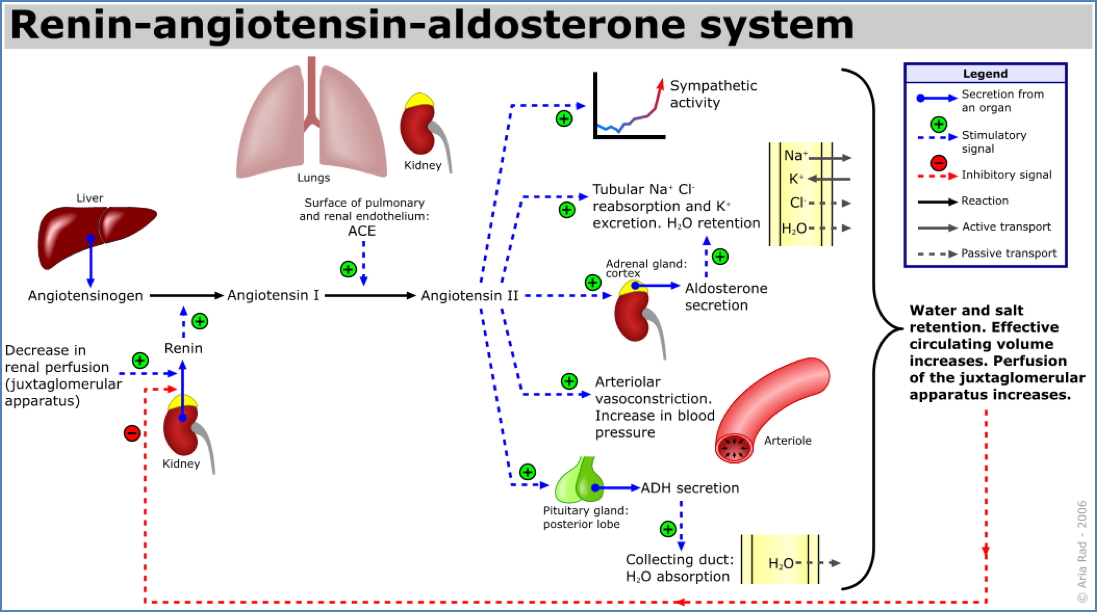
- Renin-Angiotensin-Aldosterone System blockers: ↓ Vasoconstriction, ↓ fluid retention
Complications
Malignant (Accelerated) Hypertension
- Rapid ↑ in BP >200/120 mmHg
- May cause:
- Retinopathy (e.g., haemorrhages, papilloedema)
- Acute renal injury (creatinine rise)
- Cerebral symptoms (confusion, seizures)
- Management:
- Gradual BP reduction over 24–36 hours
- Target <150/90 mmHg
- Avoid overly rapid correction → ischaemia risk
Long-Term Complications
- Cardiac: LV hypertrophy, heart failure, coronary artery disease
- Renal: Nephrosclerosis, progressive CKD
- Cerebral: Intracerebral haemorrhage, vascular dementia
- Vascular: Aneurysms, aortic dissection
- Ophthalmic: Hypertensive retinopathy
Summary – Hypertension
Hypertension is a major cause of cardiovascular morbidity and mortality worldwide. It is typically asymptomatic, but leads to significant long-term complications if untreated. Accurate diagnosis, regular monitoring, and targeted therapy—starting with lifestyle modifications and progressing to pharmacological agents—are essential to preventing end-organ damage. For a broader context, see our Cardiovascular Overview page.