Table of Contents
Overview – Ischaemic Heart Disease
Ischaemic heart disease refers to myocardial dysfunction caused by an imbalance between oxygen supply and demand, usually secondary to reduced coronary perfusion. It is the leading cause of morbidity and mortality in the Western world, commonly presenting as angina, heart failure, arrhythmia, or myocardial infarction. Early recognition and management are essential in reducing long-term cardiac damage and mortality.
Definition
- Ischaemia = Inadequate blood flow → insufficient oxygen supply to tissues
- In the heart, this results in myocardial dysfunction and potentially cell death if prolonged
- Ischaemia is a flow limitation, not an oxygen limitation (that’s hypoxia)
- Prolonged ischaemia may result in infarction (irreversible cell death)
Review of Coronary Anatomy
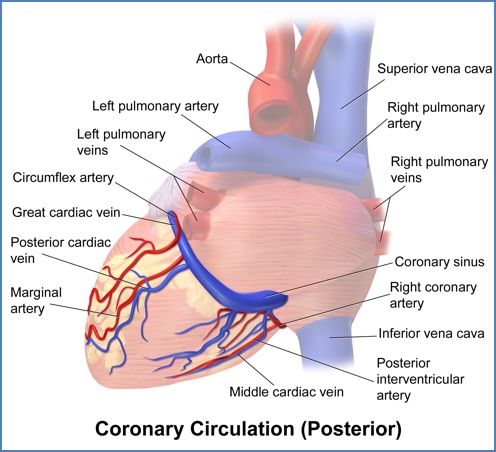
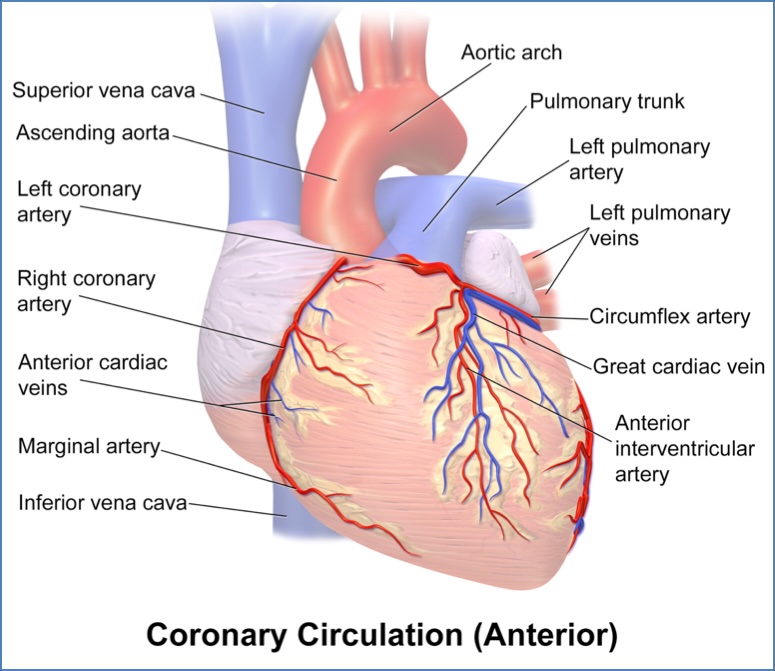
LAD → Apex, Anterior LV, Anterior 2/3 of IV-Septum
LCX → Lateral LV
RCA → Entire RV, Postero-Superior LV, Posterior 1/3 of IV-Septum
Aetiology
Causes of Decreased Oxygen Supply
- ↓ Coronary blood flow
- ↓ Aortic diastolic perfusion pressure (e.g. hypotension, aortic regurgitation)
- ↑ Coronary vascular resistance (due to vessel compression, vasospasm, or structural changes)
- ↓ O2-carrying capacity
- Anaemia
- Hypoxaemia (lung disease, CO poisoning)
- Low haemoglobin saturation or pH
Causes of Increased Oxygen Demand
- ↑ Wall tension
- ↑ Preload → ↑ myocardial stretch
- ↑ Afterload → ↑ force needed to eject blood
- ↑ Heart rate (chronotropy)
- ↑ Contractility (inotropy)
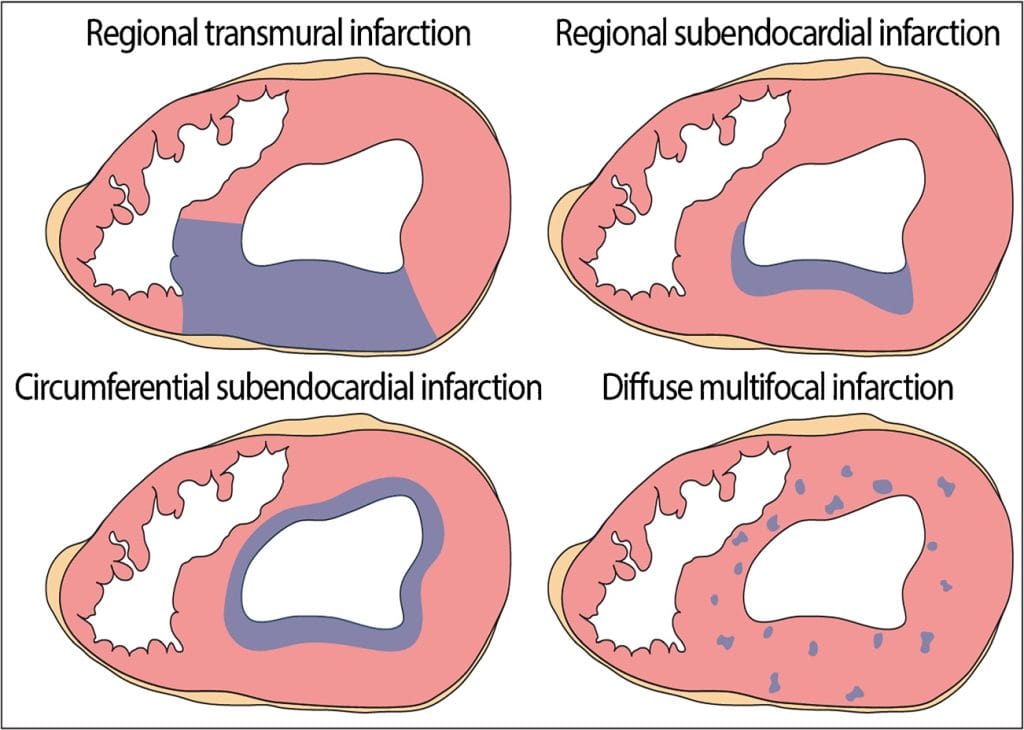
Morphology / Pathophysiology
Ischaemia vs Hypoxia vs Infarction
- Ischaemia → blood flow limitation (usually due to coronary stenosis)
- Hypoxia → oxygen delivery limitation (e.g. lung pathology)
- Infarction → irreversible necrosis due to prolonged ischaemia
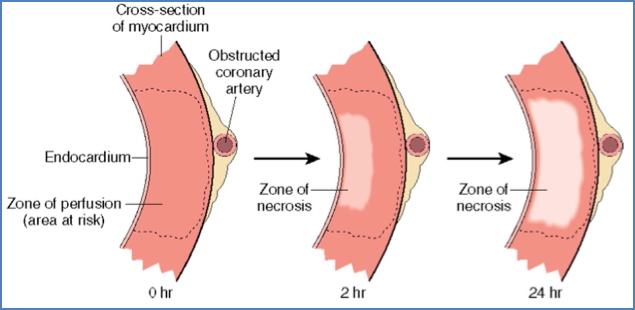
Myocardial Ischaemia
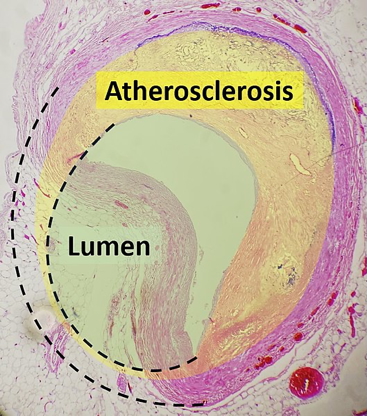
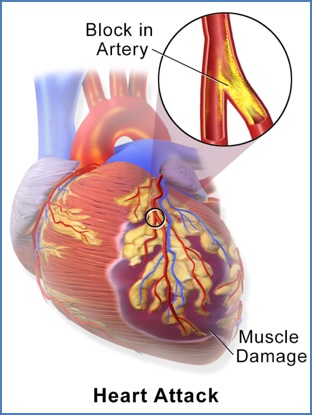
- Most commonly due to atherosclerotic plaque rupture + thrombosis
- Regional ischaemia → Localised coronary obstruction
- Global ischaemia → Rare, usually due to profound hypotension or surgical interruption
Cellular & Metabolic Effects
- ↓ ATP production → ↑ lactate, ↓ pH
- ↓ glycogen stores
- Nociceptor activation → angina
- Diastolic dysfunction → ↑ left ventricular diastolic pressure (LVDP)
- Pulmonary congestion → due to ↑ LVDP
- Reperfusion injury → oxidative stress-induced damage post-restoration of flow
- Ionic disturbances:
- ↑ intracellular Ca²⁺ → irreversible damage
- ↑ extracellular K⁺ and intracellular Na⁺ → arrhythmogenesis
Clinical Features
Degrees of Coronary Blockage
- < 70% Occlusion: Asymptomatic
- 70-75% Occlusion: Angina
- 90% Occlusion: Chronic IHD
- Unstable Plaque: Unstable angina +/- Rupture → Acute MI
- > 90% Occlusion: MI
Presentations
- Angina Pectoris
- Retrosternal chest pain due to transient ischaemia
- No necrosis (reversible)
- Stable angina: exertional, relieved by rest, ST-depression
- Prinzmetal’s angina: rest-related, vasospastic, ST-elevation
- Unstable angina: at rest, prolonged, due to plaque rupture
- Silent Ischaemia
- No pain, but abnormal ECG (e.g. ST changes)
- Ischaemic Heart Failure
- Poor myocardial function → dyspnoea, peripheral oedema
- Myocardial Infarction
- Irreversible cell death (infarct) due to persistent ischaemia
- Enzyme release (troponin I, CK-MB)
- Fibrotic, non-contractile scar formation
- 90% due to atherosclerotic plaque rupture + thrombosis
Ventricular Arrhythmias:
- Due to Myocyte Ion-Disturbances:
- ↑ Extracellular K+↑ Intracellular Na+
- ↑ Intracellular Ca+ (“Calcium-Loading”) – If Ischaemia is Prolonged → Irreversible Damage

Investigations
ECG Findings
- Subendocardial ischaemia:
- ST-depression
- T-wave inversion
- Transmural ischaemia:
- ST-elevation (seen in MI)
Diagnostic Criteria for Myocardial Infarction
Requires ≥2 of:
- Ischaemic chest pain (e.g. angina)
- Serial ECG changes (especially ST-elevation)
- Elevated serum markers (troponin, CK-MB)
Complications
- Arrhythmias → due to conduction disturbance and electrolyte shifts
- Pulmonary oedema → diastolic dysfunction and increased LVDP
- Recurrent infarction or progression to heart failure
- Pericarditis or ventricular aneurysm (post-MI)
- Sudden cardiac death
Summary – Ischaemic Heart Disease
Ischaemic heart disease is characterised by an imbalance between myocardial oxygen supply and demand, leading to symptoms such as angina, arrhythmias, or infarction. Myocardial ischaemia commonly results from coronary artery disease due to atherosclerosis and thrombosis. Understanding the pathophysiological mechanisms—from metabolic shifts to ECG changes—enables timely diagnosis and management, improving patient outcomes. For a broader context, see our Cardiovascular Overview page.