Table of Contents
Overview – Arterial Vascular Examination
The arterial vascular examination is an essential OSCE skill used to assess peripheral arterial disease (PAD), critical limb ischaemia, and complications like ulceration and gangrene. It provides key insights into vascular sufficiency, perfusion status, and the presence of acute or chronic limb ischaemia. A thorough assessment of pulses, limb temperature, skin changes, and special tests such as the Buerger test or ankle-brachial pressure index (ABPI) allows for early identification of serious pathology and timely referral for intervention.
This guide presents a comprehensive approach to performing a high-yield arterial vascular examination, commonly assessed in both vascular surgery and general medicine OSCE stations.
Definition
The arterial vascular examination involves clinical assessment of the lower limb arterial system to identify signs of acute or chronic ischaemia, evaluate pulse presence and quality, and assess trophic skin changes, ulcers, or gangrene.
Preparation
- Wash hands and introduce yourself.
- Confirm name, age, and gain consent.
- Position patient supine with legs fully exposed (wear shorts).
- Look around the bed for walking aids, medications, ECGs, or signs of diabetes (e.g. insulin pens).
- Ask about limb pain, weight loss, and cardiovascular symptoms.
Inspection
- Compare both legs for swelling and symmetry.
- Look for scars (e.g. femoropopliteal bypass, angiogram entry sites, CABG leg harvest scars).
- Colour changes:
- Pale or mottled → acute ischaemia
- Black → gangrene (dry or wet)
- Fixed duskiness (non-blanchable) → non-viable limb
- Ulcers: typically on pressure areas (between toes, heel, lateral malleolus)
- Trophic changes (chronic limb ischaemia):
- Hair loss
- Shiny, thin skin
- Nail dystrophy
- Muscle wasting
- Look for amputations
Palpation
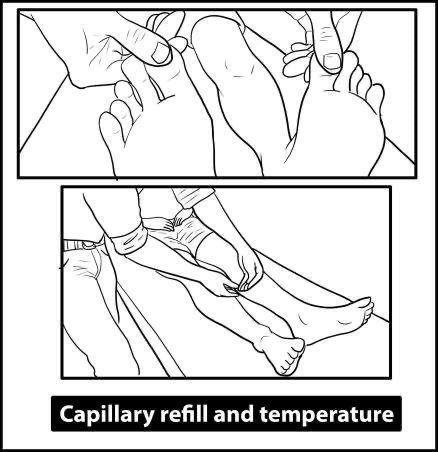
- Temperature: compare both legs with back of hand → cold = ischaemia
- Capillary refill:
- Normal < 2 seconds
- Non-blanchable = dead tissue
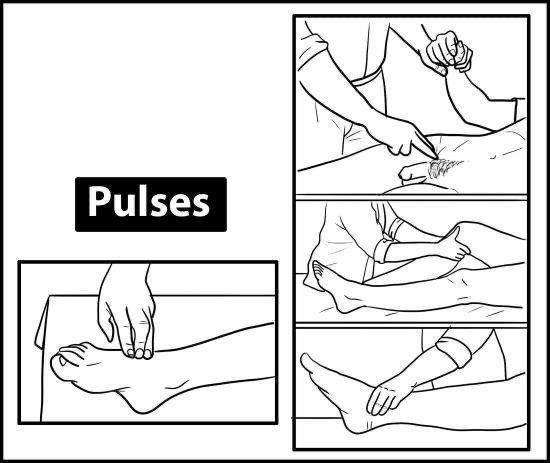
- Pulses: palpate in sequence
- Femoral artery – midpoint between ASIS and pubic symphysis
- Popliteal artery – knee flexed at 30°, hands cradling the knee
- Posterior tibial artery – behind medial malleolus
- Dorsalis pedis artery – lateral to extensor hallucis longus tendon
- If pulses are not palpable, use handheld Doppler
Auscultation
- Listen over femoral arteries and abdominal aorta for bruits, which indicate turbulent flow and possible stenosis
Sensory Testing
- Assess for paresthesia or numbness (suggests acute ischaemia)
- Perform as part of neurovascular assessment if limb is at risk
Special Tests
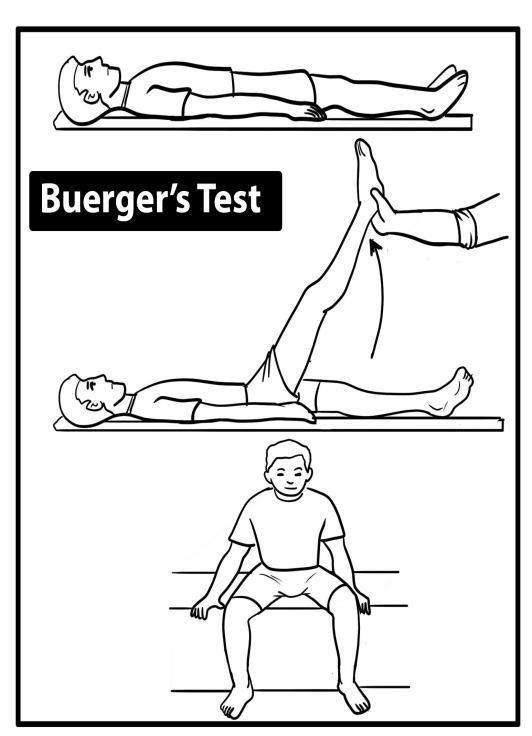
Buerger’s Test
- With patient supine, raise leg to 90°:
- Pallor at <20° → severe ischaemia
- Observe venous guttering (collapse of superficial veins)
- Sit patient up with legs dangling:
- Delayed return to pink >30 seconds = ischaemia
- Red/purple discoloration = reactive hyperaemia (chronic ischaemia)
ABPI (Ankle-Brachial Pressure Index)
- Compare systolic BP at ankle vs brachial artery:
- 0.9: Normal
- 0.5–0.9: Claudication
- 0.3–0.5: Rest pain
- <0.3: Critical ischaemia/gangrene
- Note: may be falsely high in diabetics → use Toe-Brachial Index
Clinical Syndromes
Acute Limb Ischaemia (6 Ps)
- Pain (sudden onset)
- Pallor
- Pulselessness
- Paresthesia
- Paralysis
- Perishingly cold
Causes: embolism (e.g. AF, AAA), thrombosis, trauma
Management: IV heparin, embolectomy, thrombolysis, fasciotomy if compartment syndrome develops
Chronic Limb Ischaemia
- Intermittent claudication:
- Buttock/thigh pain + erectile dysfunction → aortoiliac disease (Leriche syndrome)
- Calf pain → femoral/popliteal
- Forefoot pain → tibial/pedal arteries
- Critical limb ischaemia:
- Rest pain > 2 weeks (worse lying flat, improved when leg is dependent)
- Tissue loss (ulcer/gangrene)
- ABPI < 0.5
Ulcers – Differentiation
| Feature | Arterial | Neuropathic | Venous |
|---|---|---|---|
| Cause | Atherosclerosis, Buerger’s | Diabetes | CVI |
| Site | Tips of toes, heels | Plantar metatarsal heads | Gaiter area |
| Appearance | Small, round, punched-out | Callus border | Large, sloping edges |
| Exudate | Dry, yellow slough | Minimal | Wet, granulating |
| Sensation | Painful | Painless | Variable |
| Surrounding skin | Trophic changes | Charcot joint | Eczema, brown pigmentation |
Investigations
- Bloods: Glucose, HbA1c, lipids
- Urinalysis: Glucosuria, microalbuminuria
- ECG: Rule out AF (risk for embolism)
- Duplex ultrasound: Evaluate arterial flow
- CT angiography / MR angiography
- Exercise treadmill test
- X-ray: Rule out osteomyelitis if ulcer present
- Ulcer biopsy or swab: If infected or suspicious
Management
Lifestyle
- Smoking cessation
- Exercise therapy
- Foot care
Medical
- Antiplatelet (e.g. aspirin)
- Statins
- Blood pressure & diabetes control
Interventional
- Endovascular:
- Angioplasty ± stenting
- Thrombolysis
- Surgical:
- Embolectomy (Fogarty catheter)
- Bypass graft (e.g. femoropopliteal)
- Endarterectomy
- Amputation (for non-viable limb)
- Lumbar sympathectomy – improves rest pain when surgery contraindicated
Fontaine Classification of PAD
- I: Asymptomatic
- II: Intermittent claudication
- III: Rest pain
- IV: Ulceration/gangrene
Amputation Indications – “3 D’s”
- Dead: Gangrene, necrosis
- Dangerous: Wet gangrene, spreading cellulitis
- Damned nuisance: Non-functional limb with intractable pain
Summary – Arterial Vascular Examination
The arterial vascular examination is essential for assessing peripheral vascular disease, identifying acute or chronic limb ischaemia, and evaluating for trophic changes and ulcerations. Mastery of this skill allows early detection of limb-threatening conditions and timely vascular referral. For a broader context, see our Clinical Skills Overview page.