Table of Contents
Overview – Breast Examination
Breast examination is a vital clinical skill in OSCEs and real-world practice for evaluating breast lumps, nipple discharge, or suspicious skin changes. It plays a key role in the triple assessment of breast pathology alongside imaging and biopsy. Final-year medical students must demonstrate a confident, respectful, and systematic approach, including awareness of red flags for malignancy and metastatic disease, as well as an understanding of risk factors and staging. This article outlines a step-by-step guide for conducting a comprehensive breast exam — including inspection, palpation, lymph node assessment, and post-examination investigations.
General Principles
- Initial steps:
- Wash hands, introduce yourself, confirm name and age
- Explain the procedure clearly and obtain consent
- Offer a chaperone (always with intimate exams)
- Ask the patient to remove their top and sit upright on the bed
- Clarify the complaint:
- Ask which breast is affected — left or right?

Inspection
Around the Bed
- Look for systemic signs of metastatic disease:
- Dyspnoea, dysphonia, weight loss, jaundice, ascites, cachexia
Breast and Axilla
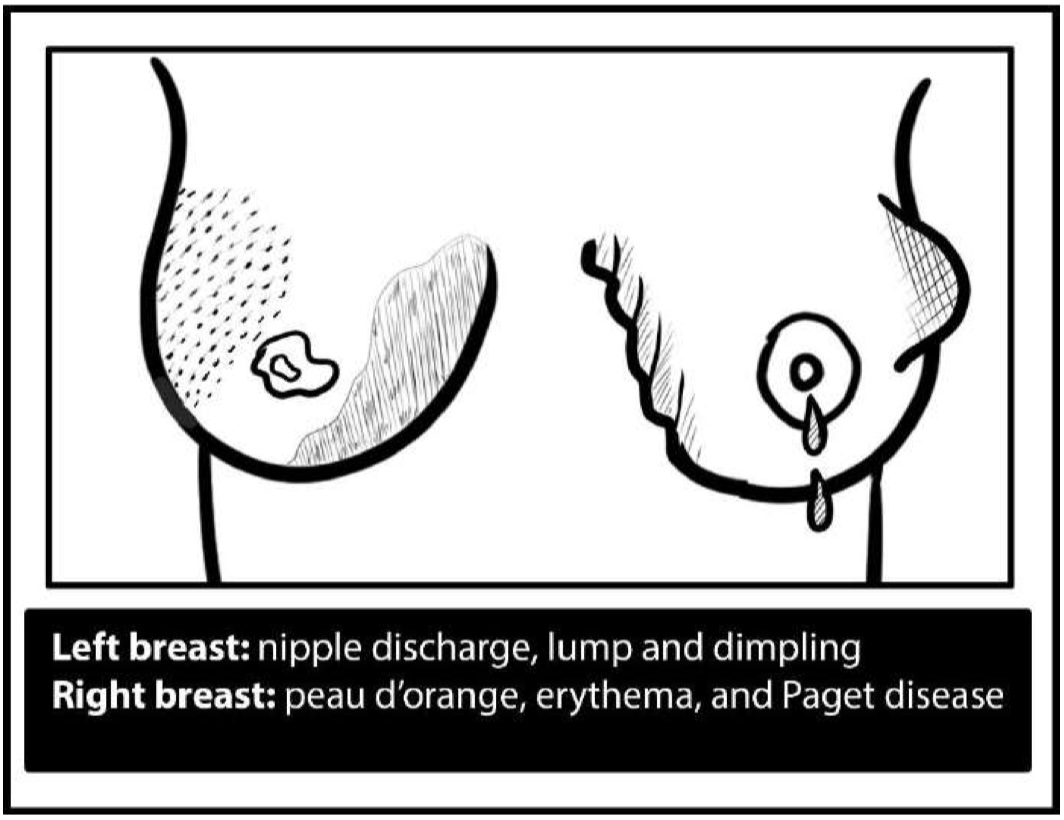
- Assess for:
- Symmetry or visible lumps
- Dimpling or skin retraction (due to Cooper’s ligament involvement)
- Skin changes:
- Ulceration (malignancy)
- Scars (e.g., post-mastectomy)
- Peau d’orange, prominent vasculature (malignancy)
- Erythema: acute mastitis or abscess
- Skin thickening with enlarged pores (cancer)
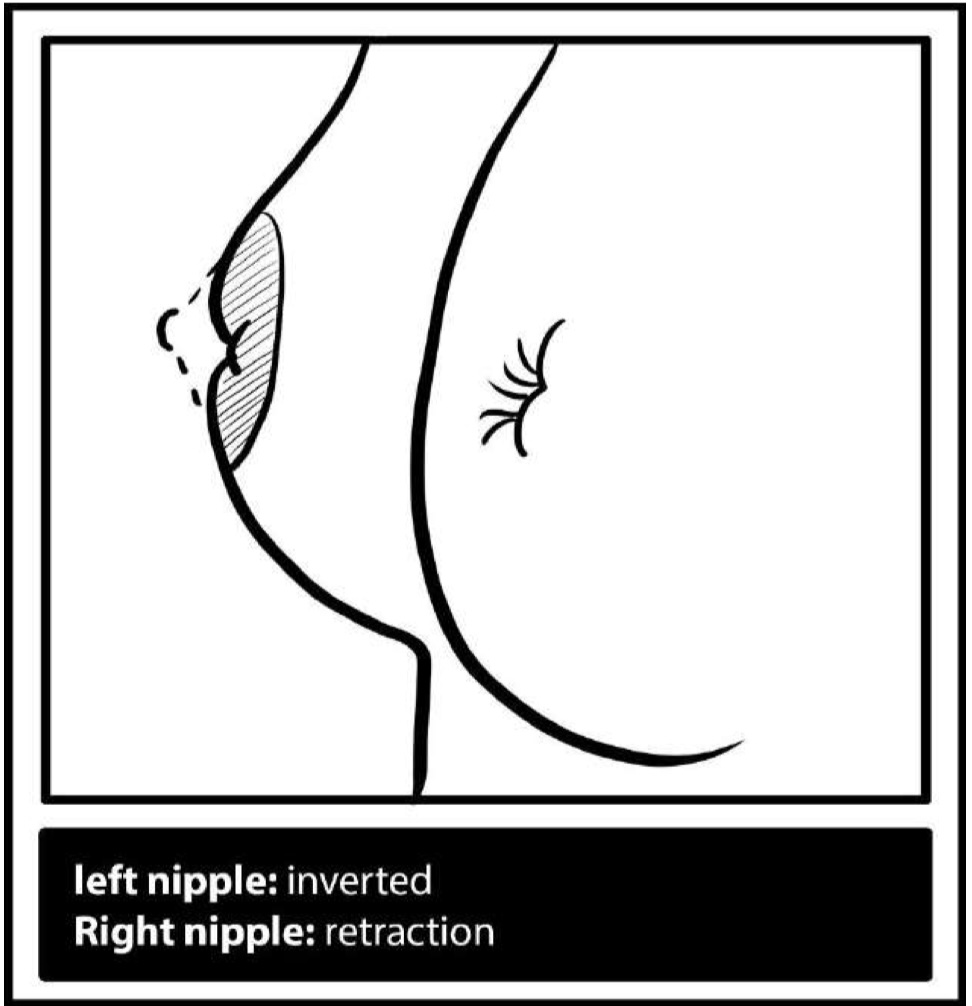
- Nipple abnormalities:
- Asymmetry, retraction, inversion
- Scaling, rash, or ulceration (Paget’s disease or eczema)
- Discharge types:
- Bloody (cancer, intraductal papilloma)
- Milky (galactorrhoea)
- Serous (fibrocystic)
- Greenish (ductal ectasia)
- Purulent (abscess)
Dynamic Inspection
- Ask the patient to:
- Press hands into hips
- Raise arms overhead
- Lean forward with arms raised
→ to reveal asymmetry, dimpling, or retraction

Palpation
Breast
- Patient lies supine, arm on examined side placed behind the head
- Start with the unaffected breast
- Use circular motion with middle three fingers in a clockwise fashion
→ Include nipple and axillary tail - Palpation notes:
- Light and deep palpation
- If a lump is found → assess:
- 4 S’s: Site, Size, Shape, Surface
- 4 T’s + FCM:
- Tenderness
- Temperature
- Transillumination
- Texture (Consistency)
- Fixation (skin, muscle, chest wall)
- Mobility
Nipple
- Gently squeeze for discharge
→ Send any fluid for cytology


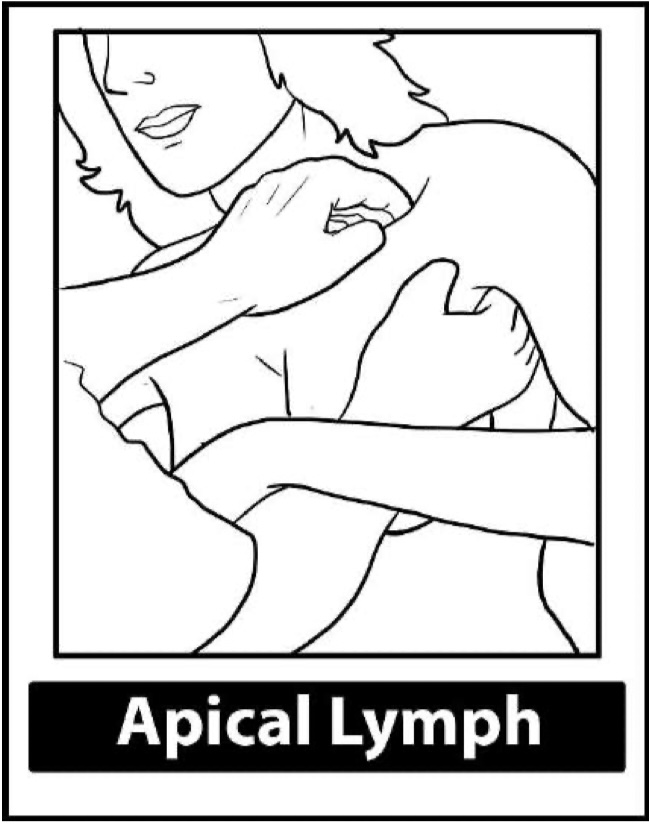
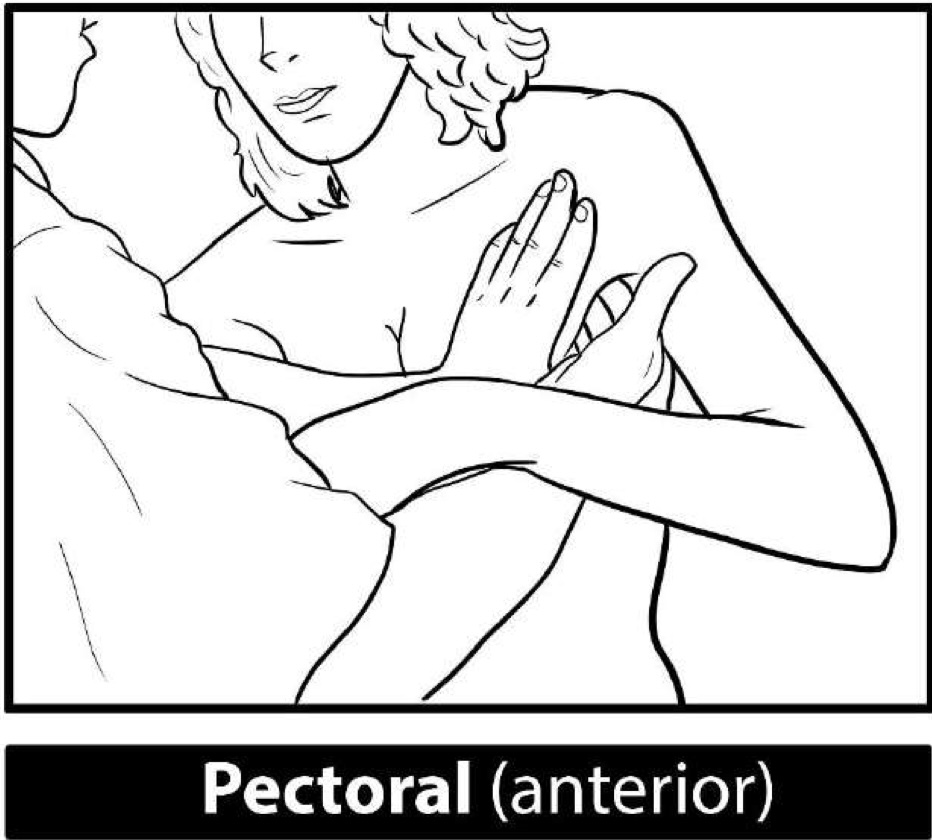
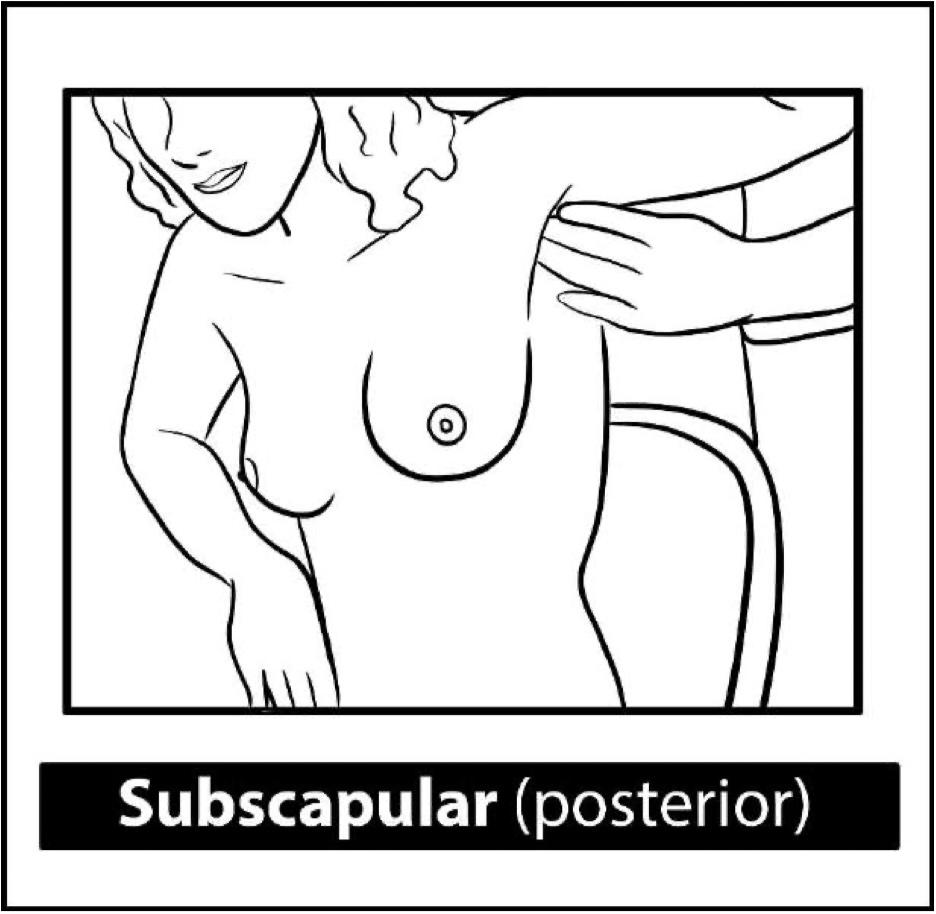
Lymph Node Examination
- Patient’s arm rested on your forearm; warn them of possible discomfort
- Axillary lymph node groups:
- Pectoral (anterior) – main breast drainage
- Subscapular (posterior)
- Humeral (lateral)
- Central (basal)
- Apical (deep in armpit, under clavicle)
- Also palpate supraclavicular and cervical nodes
Firm, non-tender, slow-growing nodes suggest malignancy

Post-Exam Assessment
Check for Metastases:
- Lungs: pleural effusion, consolidation
- Liver: hepatomegaly
- Spine: tenderness
Investigations:
- Bloods: LFTs, serum calcium
- Imaging: CXR, abdominal US, bone scan
- Ovary: transvaginal US (Krukenberg tumour)
Lymphatic Drainage
- Lateral drainage → Axillary nodes (Levels I–III relative to pectoralis minor)
- Medial drainage → Internal mammary nodes
Triple Assessment
- Clinical Exam
- Imaging:
- Mammogram: ≥35yo; look for microcalcifications, spiculated masses
- US: <35yo; solid = cancer, cyst = smooth
- MRI: high-risk, dense breasts
- Biopsy:
- FNAC: C1–C5 grading
- Core biopsy: distinguishes in situ from invasive carcinoma
Differential Diagnosis
| Condition | Features |
|---|---|
| Fibrocystic changes | Bilateral, cyclic pain, rubbery |
| Fibroadenoma | Mobile, firm, <5 cm, young women |
| Cancer | Irregular, firm, fixed, painless |
| Others: | Lipoma, cyst, phyllodes tumour, fat necrosis |
Types of Breast Cancer
Non-Invasive:
- Ductal carcinoma in situ (DCIS): comedo necrosis
- Lobular carcinoma in situ (LCIS): bilateral, impalpable
Invasive:
- Ductal (commonest), Lobular, Mucinous, Medullary, Inflammatory (peau d’orange)
Prognosis
- Nottingham Prognostic Index = (0.2 × tumour size cm) + node score + grade
- TNM staging, Bloom-Richardson grading
- Her2 overexpression, ER/PR negativity, high Ki-67 = worse prognosis
- Triple-negative cancers → aggressive, high recurrence
Treatment
Surgery
- Breast-Conserving Surgery (BCS):
- Lumpectomy + radiation (for <4cm, unifocal)
- Mastectomy:
- Simple, skin/nipple-sparing, modified radical (Patey’s), radical (includes pectoralis minor)
- Complications: lymphedema, nerve injury, pain syndrome
Reconstruction
- Immediate or delayed
- Implants (Becker), flaps (DIEP, TRAM, LD)
Chemotherapy
- Neoadjuvant for large, node-positive, or metastatic
- Regimens: CMF, CAF, MMM
- SEs: alopecia, nausea, marrow suppression
Hormonal Therapy
- HER2+: Trastuzumab (check echo – risk of CHF)
- ER/PR+:
- Premenopausal: Tamoxifen ± oophorectomy
- Postmenopausal: Aromatase inhibitors (e.g., anastrozole)
Radiotherapy
- Indicated post-BCS, large tumours, or lymph node involvement
Lymph Node Management
- Sentinel node biopsy → Axillary clearance if >2mm metastasis
- Prevent lymphedema: elevation, compression, avoid BP cuffs
Metastasis
- Bone: bisphosphonates, radiotherapy
- Pleural effusion: drainage
- Brain/liver: directed radiotherapy or chemotherapy
Summary – Breast Examination
The breast examination is a core OSCE skill that requires a respectful, systematic approach, with attention to signs of malignancy, lymph node involvement, and metastatic spread. It plays a crucial role in the triple assessment, guiding further imaging and biopsy. Understanding the types of breast cancer, staging systems, and treatment options is essential for clinical competency. For a broader context, see our Clinical Skills Overview page.