Table of Contents
Overview – Ear Examination Guide
The ear examination guide is an essential clinical skill for assessing hearing complaints and diagnosing outer, middle, and inner ear pathology. By inspecting the external structures, performing otoscopy, and using tuning fork tests like Weber and Rinne, clinicians can distinguish between conductive and sensorineural hearing loss. This guide provides a step-by-step approach for final-year medical students, ensuring they can confidently examine the ear and interpret key findings in OSCE or clinical settings.
History Taking – Ear Symptoms
Presenting Complaints
History of Presenting Complaint
- Onset: Sudden, gradual, intermittent
- Laterality: Unilateral or bilateral
- Duration: Hours, days, weeks
- Aggravating/relieving factors: Noise exposure, positioning, movement
- Associated symptoms: URTI, fever, facial nerve symptoms
- Recent history: Loud noise, barotrauma, trauma
Past Medical History
- Birth complications (hypoxia, low birth weight <1500g)
- Craniofacial abnormalities
- Genetic syndromes (e.g. Meniere’s disease)
- Chronic or recurrent infections (ear, sinus, URTI)
- Previous trauma or surgery
Surgical History
- Grommet insertion
- Sinus, head, or neurosurgery
Medications
Ototoxic drugs:
- Aminoglycosides (e.g. Gentamicin)
- High-dose aspirin
- Chemotherapeutics
Social History
- Occupational/recreational noise exposure
- PPE usage
Family History
- Hereditary hearing loss
- Genetic conditions
External Ear Examination
Inspection
- Assess skin: Colour, texture, lesions (e.g. moles, cysts, nodes, deformities)
- Look for cancer signs: Basal cell carcinoma, melanoma
- Check for redness or swelling
- Assess discharge: Note colour and odour
Palpation
- Gently palpate for pain, tenderness, texture changes, or lesions
- Pain ↑ on movement → Suggests otitis externa
- No pain change → More likely otitis media
- Mastoid tenderness → Suspect mastoiditis
Otoscopy Technique
Preparation
- Use largest comfortable speculum
- Always examine the unaffected ear first
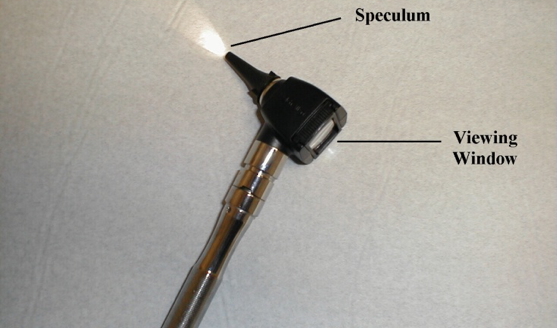
Procedure
- Place speculum at external canal entrance
- Gently pull pinna upward and backward
- Insert otoscope slowly, angled slightly toward the nose
- Observe external canal:
- Normal = spacious, healthy walls
- Otitis externa = red, swollen, narrowed canal

Tympanic Membrane Examination
What to Look For
- Colour: Normal is greyish, translucent
- Landmarks (visible through membrane):
- Malleus handle (Hm), Umbo (Um), Light reflex (Lr)
- Annulus fibrosis (An), Lateral process of malleus (Lp)
- Pars flaccida (Attic) (At), Long process of incus (Lpi – occasionally visible)


Pathological Signs
- Diffuse redness → Otitis media
- Bulging membrane with loss of light reflex → Middle ear effusion
- Perforation or scarring may also be noted
Hearing Assessment Tests
Conductive vs Sensorineural Loss
- Conductive hearing loss: Obstruction of sound through external or middle ear
- Sensorineural hearing loss: Dysfunction of the cochlea or auditory nerve (CN VIII)
Weber Test
- Place vibrating tuning fork stem towards the back of the patient’s head or on forehead, equidistant from either ear. The bones of the skull will transmit this sound to the 8th nerve, which should then be appreciated in both ears equally.
- Interpretation:
- Lateralises to affected ear → Conductive loss
- Lateralises to normal ear → Sensorineural loss
- Heard equally → Normal or bilateral loss

Rinne Test
- Step 1: Place fork base on mastoid bone
- Step 2: When no longer heard, move to just outside canal
- Interpretation:
- Normal: Air conduction > Bone conduction (Rinne positive)
- Conductive loss: Bone ≥ Air (Rinne negative)
- Sensorineural loss: Both reduced, but Air still > Bone (Rinne positive)

Summary – Ear Examination Guide
The ear examination guide provides a systematic approach to diagnosing ear conditions. Through careful inspection, otoscopy, and bedside tests like Weber and Rinne, students can effectively assess hearing loss and localise the pathology. For a broader context, see our Clinical Skills Overview page.