Table of Contents
Overview – Eye Examination
The eye examination is a vital clinical skill for assessing visual symptoms, diagnosing ocular and systemic disease, and detecting red flags that may require urgent referral. A large proportion of diagnoses are made from history alone, making a structured and focused approach essential. This guide covers key components including symptom analysis, physical signs, visual testing, and fundoscopy—crucial knowledge for OSCE stations and clinical rotations.
History Taking
Presenting Complaints
Determine the nature of the symptom:
- Abnormal Vision
- Reduced Vision
- Central or peripheral?
- Sudden onset suggests vascular causes
- Scotoma: Localised visual field loss
- Hemianopia: Bitemporal (optic chiasm lesion)
- Night Blindness: Often due to vitamin A deficiency
- Colour Blindness: X-linked recessive, affects 8% males
- Floaters: Suggest haemorrhage or vitreous degeneration
- Flashing Lights: Unilateral = retinal, Bilateral = migraine
- Haloes: Suggest increased intraocular pressure
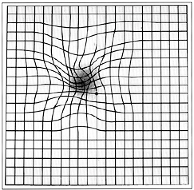
- Metamorphopsia / Micropsia: May indicate macular degeneration
- Diplopia (Double Vision)
- Binocular: Muscle/nerve issues
- Monocular: Structural or cortical causes
- Reduced Vision





- Abnormal Sensation
- Foreign Body Sensation: Trichiasis, conjunctivitis, dry eye
- Achy Pain: Photophobia, iritis, keratitis
- Severe Deep Pain: Closed-angle glaucoma, herpes zoster
- Asthenopia (Eye Strain): Refractive error or heterophoria
- Watery Eyes/Discharge: Overproduction or faulty drainage
- Altered Appearance
- Proptosis: Trauma, mass, thyroid disease
- Ptosis: CN III palsy, lid disorders
- Lid Retraction: Graves’ disease
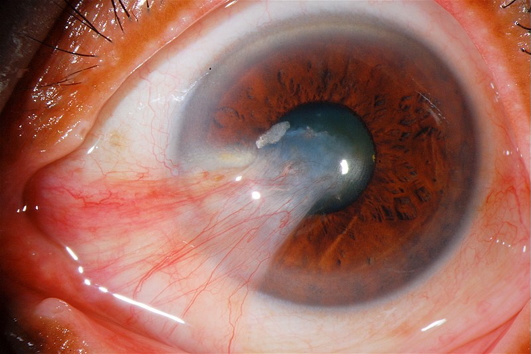
- Lesions: On lids or globe (e.g. pterygium)
- Redness, Ciliary injection, Corneal opacities

http://kellogg.umich.edu/theeyeshaveit/common/proptosis.html

Andrewya, Public domain, via Wikimedia Commons

Jonathan Trobe, M.D. – University of Michigan Kellogg Eye Center, CC BY 3.0
Jmvaras, CC BY-SA 4.0


Additional History
- Medications, allergies, diabetes
- Occupational exposures (e.g. welders)
- Family and social history
General Inspection
- Visual aids (glasses, patches), mobility aids (guide dog, cane)
- Check for systemic clues (e.g. tremor, skin signs)
Vital Signs
- Pulse: Irregularity (e.g. atrial fibrillation → amaurosis fugax)
- BP: Hypertension → retinopathy
- RR & Temp: Raised in infection
Visual Acuity
- Use Snellen chart, check each eye separately with correction
- Use pinhole if acuity is poor → corrects refractive errors
- Note blind spot enlargement (e.g. papilloedema, macular degeneration)
Colour Vision
- Use Ishihara plates
- Common in red-green blindness (X-linked)
External Eye Inspection
Eyelids
- Lid retraction or lag (Graves’)
- Ptosis (Horner’s, CN III palsy)
- Periorbital oedema (nephrotic syndrome, allergies)
- Xanthelasma (lipid disorders)
- Skin lesions (SCC, BCC)
- Eyelash abnormalities (trachoma)
Eyeball
- Exophthalmos (thyroid, tumour)
- Enophthalmos (dehydration, trauma)
Conjunctiva
- Pallor (anaemia), icterus (liver disease), haemorrhages
- Conjunctivitis = redness + discharge
Iris, Cornea, Lens
- Arcus senilis (CVD risk)
- Kayser-Fleischer ring (Wilson’s disease)
- Band keratopathy (hypercalcaemia)
- Cataracts (diabetes, iodine deficiency)
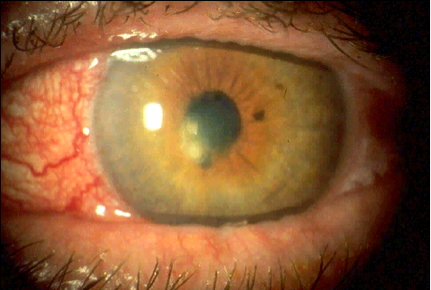
- Corneal ulceration (herpes, trachoma)
- Hypopyon/hyphaema (pus or blood in anterior chamber)
Pupillary Reflexes
- Check size (normal 2.5–3.5 mm)
- Direct and consensual light response
- Swinging torch test → Marcus-Gunn pupil = relative afferent pupillary defect
Visual Fields
- Confrontation testing, one eye at a time
- Common field defects:
- Bitemporal hemianopia: Optic chiasm lesion
- Homonymous hemianopia: Optic radiation lesion
- Unilateral field loss: Optic nerve lesion
- Enlarged blind spot = papilloedema
Eye Movements
- Assess all directions
- Cranial nerve control:
- CN III → most muscles
- CN IV → superior oblique
- CN VI → lateral rectus
- Note diplopia or nystagmus (cerebellar signs)
Fundoscopy
- Papilloedema
- Macular degeneration
- Diabetic and hypertensive retinopathy
- Roth spots (infective endocarditis)
Summary – Eye Examination
The eye examination combines careful history with inspection, acuity tests, field checks, and fundoscopy to diagnose ocular or systemic disease. It’s crucial for recognising red flags like glaucoma, retinal detachment, or vascular occlusions. For a broader context, see our Clinical Skills Overview page.