Table of Contents
Overview – Hernia & Stoma Examination
The hernia and stoma examination is an essential part of gastrointestinal (GIT) and surgical OSCE stations. It tests a candidate’s ability to identify abdominal wall hernias, evaluate their characteristics, and assess surgical stomas including their type, location, and potential complications. This examination provides crucial diagnostic information in both elective and emergency settings — especially for identifying strangulated or obstructed hernias and evaluating surgical recovery following colostomy or ileostomy procedures.
This article presents a structured, high-yield approach to hernia and stoma examination, including inspection, palpation, special tests, differential diagnosis, and associated pathologies.
Definition
- Hernia: Protrusion of an organ or tissue through a defect in the wall of the cavity that normally contains it.
- Stoma: A surgically created external opening from the intestine or urinary tract onto the abdominal wall to divert flow.
Examination Preparation
- Wash hands, introduce yourself, obtain consent.
- Ensure full exposure of the abdomen and groin.
- Position the patient supine and later standing if needed.
Hernia Examination
Inspection
- Scars: Suggest incisional hernia
- Obvious swelling or lumps
- Skin changes: erythema (suggests strangulation)
- Scrotal swelling: may suggest indirect inguinal hernia
- Ask patient to cough – observe for visible impulse (cough impulse)
- Ask patient to stand if lump is not visible when lying
Palpation
- Location:
- Inguinal: Superomedial to pubic tubercle
- Femoral: Infralateral to pubic tubercle
- Cough Impulse Test:
- Place fingers over suspected site
- Ask patient to cough and feel for impulse
- Absent in strangulated or femoral hernias
- Reducibility:
- Gently reduce with patient supine
- Apply pressure to midpoint of inguinal ligament → ask patient to cough:
- Swelling reappears → Direct hernia
- No reappearance → Indirect hernia
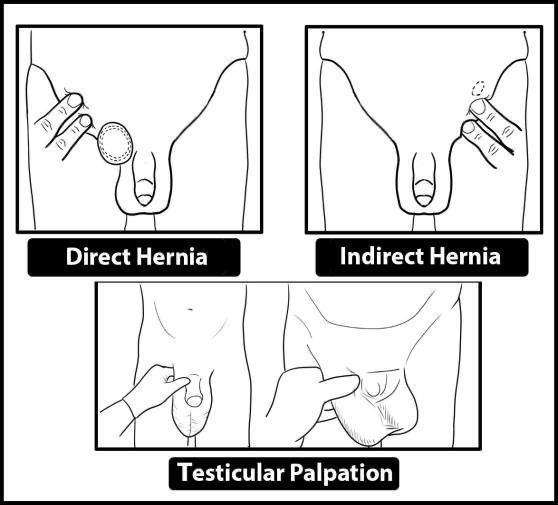
- Zieman’s Three-Finger Test:
- Index: Internal ring (indirect)
- Middle: External ring (direct)
- Ring: Femoral canal (femoral)
- Cough to localise hernia origin
- Scrotal Palpation:
- Examine for extension of indirect inguinal hernia
Percussion and Auscultation
- Percussion:
- Resonant → bowel
- Dull → omentum
- Auscultation:
- Bowel sounds → suggests gut content
- Absent → possible strangulation or omental content
Hernia Types and Characteristics
Inguinal Hernias
- Indirect:
- Through internal ring into scrotum
- Lateral to inferior epigastric vessels
- Common in young males
- Direct:
- Medial to inferior epigastric vessels
- Through Hesselbach’s triangle
- Common in older males, bilateral, often reducible
Femoral Hernia
- Below inguinal ligament
- High risk of strangulation
- Common in females
- May be tender and irreducible
Other Hernias
- Incisional: Through surgical scars
- Epigastric: Through linea alba above umbilicus
- Paraumbilical: Near umbilicus; high risk of strangulation
- Umbilical: Congenital or due to ascites; everted umbilicus
- Spigelian: Lateral to rectus muscle; below umbilicus

Complications
- Irreducible: Cannot be returned to cavity
- Obstructed: Contents obstructed, but blood supply intact
- Strangulated: Compromised blood supply → surgical emergency
- Richter’s hernia: Only part of bowel wall trapped
Stoma Examination
General Steps
- Continue from GIT exam
- Use gloves and check for patient discomfort
Inspection – LLSSCCC
- Location: RIF (ileostomy), LIF (colostomy), flank (urostomy)
- Lumen: Number of lumens (single or double)
- Spout: Spouted (ileostomy, urostomy) vs flush (colostomy)
- Skin: Inflammation, pyoderma gangrenosum
- Contents: Liquid (ileostomy), solid (colostomy), urine (urostomy)
- Complications: Retraction, prolapse, stenosis, hernia
Palpation & Auscultation
- Use two fingers to assess for:
- Cough impulse (parastomal hernia)
- Tenderness
- Auscultate for bowel sounds → tinkling in obstruction
Ask the Patient
- “Is the anus still present?” – If not, suspect abdominoperineal resection
- Look for:
- Pedicled VRAM flap in perineal area
- Previous surgeries and scars
Types of Stomas
| Type | Location | Features | Indications |
|---|---|---|---|
| End Colostomy | LIF | Single lumen, flush | Hartmann’s, rectal cancer |
| Loop Colostomy | Above umbilicus | Two lumens, temporary | Diverticulitis, obstruction |
| Double-Barrelled Colostomy | LIF | Two separate lumens | Temporary diversion |
| End Ileostomy | RIF | Spouted, liquid stool | Total colectomy, FAP, UC |
| Loop Ileostomy | RIF | Two lumens | Temporary – protect distal anastomosis |
| Urostomy | Varies | Spouted, urine output | Cystectomy, neurogenic bladder |
Management of Hernias
- Conservative:
- Truss for patients unfit for surgery
- Surgical repair:
- Lichtenstein repair – Mesh-based (open)
- Shouldice repair – No mesh
- Laparoscopic – TAPP or TEP for bilateral/recurrent
Femoral Hernia Approaches
- Lockwood – Below inguinal ligament
- Lotheissen – Through inguinal canal
- McEvedy – Above inguinal canal
Post-op Complications
- Pain, neuralgia
- Hematoma, infection
- Ischaemic orchitis
- Scrotal swelling
- Recurrence
Summary – Hernia & Stoma Examination
The hernia and stoma examination is a critical clinical skill in OSCEs and surgical assessment. It focuses on identifying hernia types, assessing reducibility and complications, and evaluating stomas for function and pathology. A thorough understanding of hernia anatomy and stoma variations supports accurate diagnosis and patient management. For a broader context, see our Clinical Skills Overview page.