Table of Contents
Overview – The Cardiovascular Examination
The cardiovascular examination is a cornerstone clinical skill that enables medical students and doctors to identify signs of heart disease and circulatory dysfunction. This comprehensive, systematic exam includes inspection, palpation, percussion (when indicated), and auscultation across the hands, face, neck, chest, abdomen, and lower limbs. Mastery of the cardiovascular examination is essential in detecting conditions such as heart failure, valvular disease, infective endocarditis, and congenital syndromes.
Definition
The cardiovascular examination is a structured bedside assessment used to evaluate the function and integrity of the heart and vascular system through physical signs and symptoms.
General Inspection
- Initial Approach: Introduction, consent, hand hygiene.
- Body Habitus:
- Cardiac cachexia → Suggests advanced heart failure.
- Obesity → Risk factor for diabetes, dyslipidaemia, hypertension.
- Level of Consciousness: Alertness and orientation.
- Respiratory distress → May indicate congestive cardiac failure, pulmonary hypertension, cor pulmonale, myocardial infarction.
- Pain/Discomfort → Consider angina, myocardial infarction, pericarditis, cardiac tamponade.
- Diaphoresis → Often associated with cardiac ischemia.
- Chest Scars/Deformities:
- Sternotomy scars → Coronary artery bypass graft (CABG), valve surgery.
- Syndromic Facies:
- Marfan’s, Down’s, Turner’s syndrome → Clues to congenital heart disease.

Vital Signs
- Pulse:
- Tachycardia → Shock, MI, pain, anaemia.
- Irregular rhythm → Atrial fibrillation (may be secondary to MI, alcohol use, or valvular disease).
- Low-volume pulse → Shock, MI, tamponade.
- Respiratory Rate: Tachypnoea suggests shock or anaemia.
- Blood Pressure:
- Hypertension → Essential, pain-induced.
- Hypotension → Shock, advanced heart failure.
- Temperature:
- Fever → Infective endocarditis, pericarditis, myocarditis.
Hands
- Peripheral Circulation: Capillary refill time (CRT).
- Colour Changes:
- Pale nails, palmar crease pallor → Anaemia.
- Peripheral cyanosis → Heart failure.
- Palmar erythema → Polycythaemia.
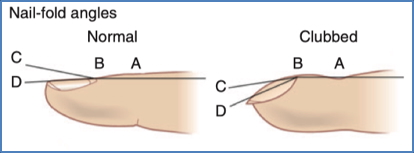
- Clubbing:
- Seen in chronic hypoxia (e.g. cyanotic congenital heart disease).

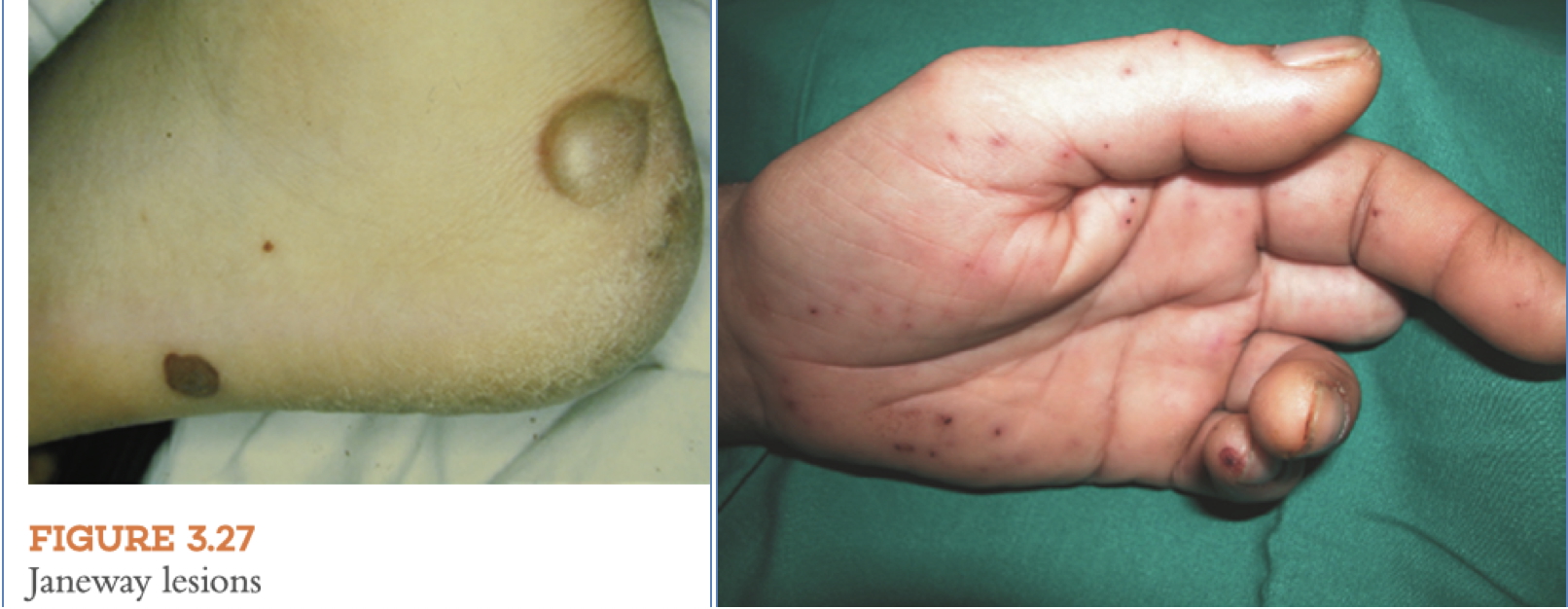
- Infective Endocarditis Signs:
- Splinter haemorrhages.
- Osler’s nodes → Painful, on fingertips.
- Janeway lesions → Painless, on palms.

- Metabolic Indicators:
- Xanthomata → Hyperlipidaemia.
- Dupuytren’s contracture → Linked to alcohol use; can reflect dilated cardiomyopathy.
Arms
- Pulse Timing Delays:
- Radio-radial delay → Coarctation of the aorta.
- Radio-femoral delay → Also suggests coarctation.
- Track Marks:
- Intravenous drug use → Risk for infective endocarditis.


Face
- Eyes:
- Conjunctival pallor → Anaemia.
- Scleral icterus → Hepatic congestion or haemolysis.
- Xanthelasma → Lipid disorder.
- Arcus senilis → Cardiovascular risk.
- Fundoscopy → Roth spots (infective endocarditis).




- Malar Appearance:
- Mitral facies → Seen in mitral stenosis.
- Mouth:
- Hydration status.
- Central cyanosis → Congestive heart failure.
- Gum pallor → Anaemia.
- Poor dentition → Risk for infective endocarditis.
- High arched palate → Marfan syndrome.
Neck
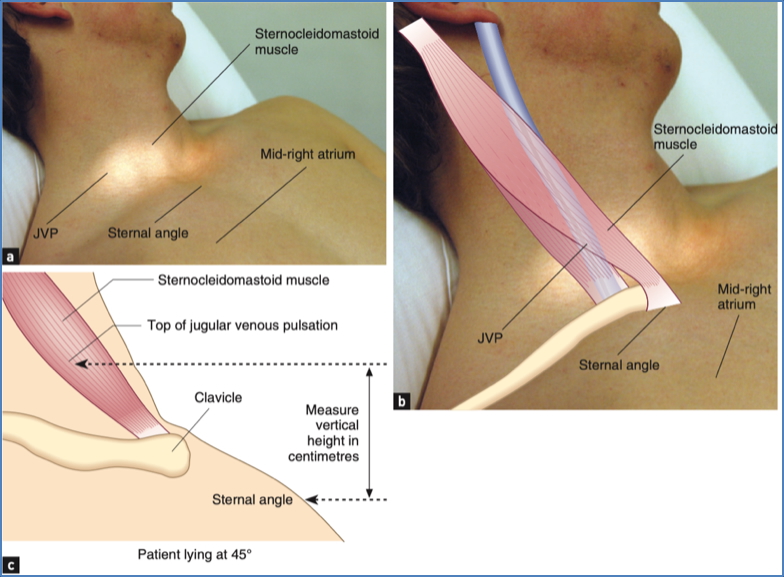
- Jugular Venous Pressure (JVP):
- Elevated in right heart failure or pulmonary hypertension.
- Hepatojugular reflux can confirm JVP rise.
- Carotid Pulses:
- Volume and character (e.g. bounding, thready).
- Carotid bruits → Suggest carotid artery stenosis.
Chest
- Inspection:
- Scars → Sternotomy from CABG/valve repair.
- Deformities → Pectus excavatum/carinatum, kyphosis.
- Pacemakers and visible apex beat.
- Palpation:
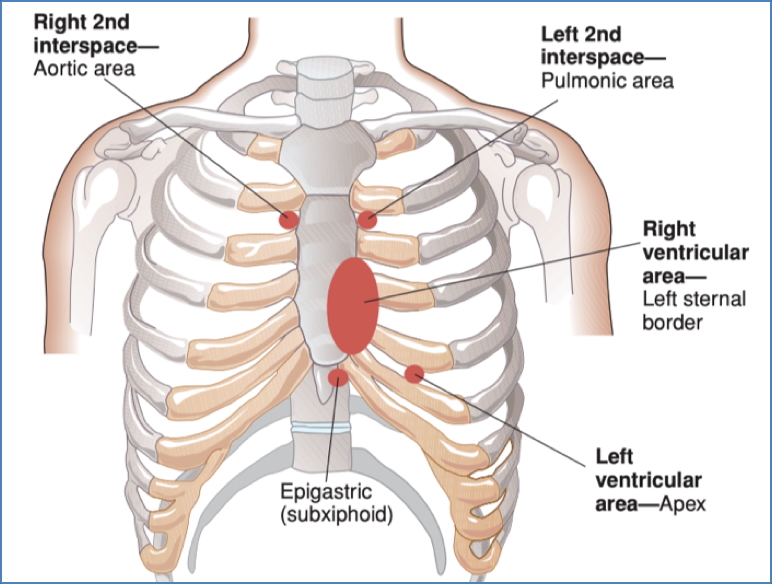
- Apex beat → Normally 5th intercostal space midclavicular line.
- Displaced → Cardiomegaly or hypertrophy.
- Heaves → Suggest ventricular hypertrophy.
- Thrills → Palpable murmurs.
- Apex beat → Normally 5th intercostal space midclavicular line.
- Auscultation:
- Muffled heart sounds → COPD or tamponade.
- Murmurs:
- Diastolic → Use bell.
- Systolic → Use diaphragm.
- Radiation → Carotids or axilla.
- Pericardial rub → Suggests pericarditis.
Back
- Respiratory Signs:
- Basal crackles → Left-sided heart failure.
- Sacral Oedema:
- Suggests fluid overload or right-sided failure.
Abdomen
- Pulsatile Masses: Abdominal aortic aneurysm.
- Scars/Tenderness
- Hepatomegaly:
- Passive congestion (RHF); pulsatile in tricuspid regurgitation.
- Splenomegaly: Infective endocarditis.
- Ascites:
- Fluid overload due to RHF.
- Renal Bruits: Renovascular hypertension.
Legs & Feet
- Peripheral Oedema:
- Bilateral → Right heart failure or fluid retention.
- Venous Stasis Signs:
- Hair loss, shiny skin, venous ulcers.
- Arterial Signs:
- Ulcers, cold limbs, reduced pulses (popliteal, dorsalis pedis, posterior tibial).
- Capillary Refill/Perfusion
- Clubbing & Endocarditis Signs:
- Repeat inspection for splinter haemorrhages, Janeway lesions, Osler’s nodes.


Summary – The Cardiovascular Examination
The cardiovascular examination is a vital clinical skill used to identify signs of cardiac disease including heart failure, valvular dysfunction, and infective endocarditis. It involves a detailed inspection of systemic signs from the hands and face to the chest, abdomen, and legs, and integrates palpation and auscultation findings to form a diagnostic impression. For a broader context, see our Clinical Skills Overview page.