Table of Contents
Overview – The Preoperative Assessment
The preoperative assessment is a structured, multidisciplinary process that ensures patient safety and optimises outcomes before surgery. It identifies potential anaesthetic and surgical risks, manages comorbidities, ensures informed consent, and streamlines perioperative planning. Final-year medical students must understand this comprehensive approach to assess readiness for surgery, minimise complications, and improve patient outcomes in the perioperative period.
Identity & Consent Verification
- Patient Confirmation: Confirm identity, procedure, and side
- Ask: “What operation are you having today?”
- Ensure the correct side is clearly marked
- A “time out” will occur in theatre to confirm identity, site, and procedure
- Informed Consent
- Ensure capacity and understanding
- Consent is not a contract and can be withdrawn at any time
- Risks are relative; benefit must outweigh harm
- Anaesthetic Risks:
- Atelectasis
- Pneumothorax
- Pneumonia
- Aspiration
- Mouth injury
- Sore throat
- Awareness
- Coma
- Malignant hyperthermia (→ rhabdomyolysis, usually fatal)
- Anaphylaxis
- Cardiac arrest, death
- Surgical Risks:
- Bleeding and transfusion reactions
- Infection and wound complications
- DVT and pulmonary embolism
- Disability, nerve palsy
- Death
- Procedure-Specific Risks (examples):
- Brain damage (Neurosurgery)
- Stroke (Carotid Endarterectomy)
- Hypothyroidism / Hypoparathyroidism (Thyroidectomy)
- CBD injury (Cholecystectomy)
- Ileus and adhesions (Abdominal surgery)
Anaesthetic Risk Assessment
- Cardiorespiratory evaluation
- Comorbidities:
- Ischaemic heart disease
- Hypertension
- Diabetes mellitus
- Asthma/COPD
- Epilepsy
- Liver/renal disease
- Pregnancy
- Other considerations:
- Allergies
- Smoking status
- Previous anaesthesia or complications
- Family history of malignant hyperthermia
Medication Review
- Steroid use
- May need IV hydrocortisone (50–100 mg) pre-op and TDS for up to 3 days
- Anticoagulants
- Oral Contraceptive Pill / Hormone Replacement Therapy
- Stop 4 weeks pre-op (esp. major/leg surgery) due to DVT risk
- Resume 2 weeks post-op
Preoperative Checklist
- Fasting:
- No solids ≥6 hours pre-op
- Clear fluids up to 2 hours pre-op
- Cannula and catheter (if indicated)
- Group & Screen/Crossmatch
- Group & Hold (e.g. cholecystectomy)
- Crossmatch 2U (Caesarean), 4U (Gastrectomy), 6U (AAA repair)
- Routine bloods:
- FBC (check Hb)
- U&E (esp. in diabetes, renal/liver disease, TPN)
- Targeted tests:
- LFTs (if jaundiced/malignancy)
- Amylase (acute abdomen)
- Drug levels (e.g. digoxin, lithium)
- TFTs (thyroid disease)
- Other tests:
- CXR (if >65, cardiac/resp Hx, mets risk)
- ECG (if >55 or cardiac risk factors)
- Book relevant imaging
DVT Prophylaxis
- Graduated compression stockings (avoid in vasculopaths)
- Heparin 5000 U SC 2 hours pre-op OR LMWH (e.g. enoxaparin 20mg SC daily)
- Continue BD post-op until ambulatory
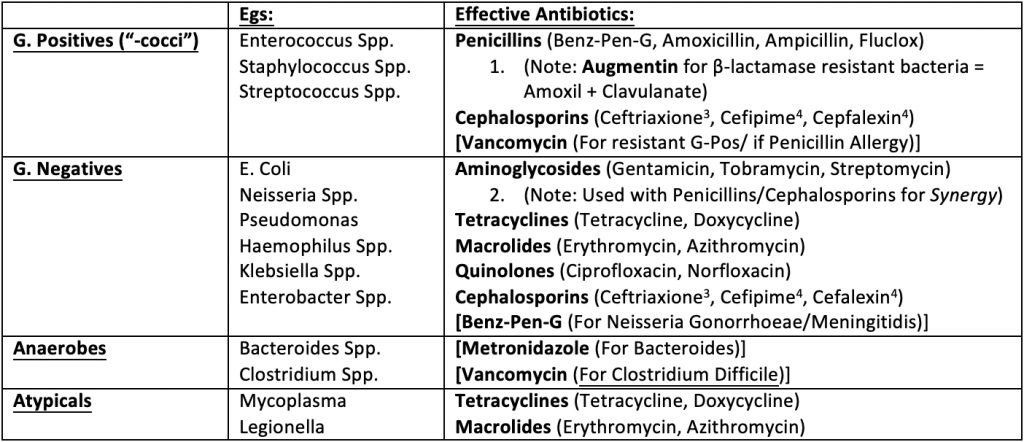
Prophylactic Antibiotics
| Procedure | Pathogens | Antibiotics |
|---|---|---|
| Appendectomy (non-perf), colorectal surgery | Enteric G–ve | Cephalexin + Metronidazole |
| Biliary/Duodenal surgery | G–ve + G+ve cocci | Cephalexin + Metronidazole |
| Ortho surgery | Staph, Strep, anaerobes | Cephalexin / Gentamicin |
| Vascular surgery | Staph, G–ve bacilli | Cephalexin / Gentamicin / Augmentin |
| Urologic surgery | G–ve bacilli, Enterococcus | Cephalexin / Ciprofloxacin |
| Gynae surgery (e.g. C-section, hysterectomy) | Staph, Strep, G–ve | Cephalexin / Gentamicin / Ampicillin |
Broad-spectrum combo: Ampicillin + Gentamicin + Metronidazole = “AGM”
Cardiovascular Pre-op Assessment
Functional Assessment
- Pump – Myocardial function
- Valves – Stenosis worse than regurgitation under load
- Pipes – Peripheral vasculature
- Control – Arrhythmias/conduction system
History
- Cardiac failure: orthopnoea, PND, oedema
- Ischaemia: angina, MI, family history
- Valvular: rheumatic fever, murmur
- PVD: claudication, smoking, diabetes
- Conduction: palpitations, blackouts
Examination
- Crepitations, displaced apex
- Heaves, murmurs
- Pulses, CRT, ulcers
- ECG for arrhythmias
- Check for previous surgery/scars
Summary – The Preoperative Assessment
The preoperative assessment is a critical step in surgical safety, encompassing patient identity checks, risk discussion, medication review, and DVT and infection prevention. Understanding comorbidities and anaesthetic risks allows clinicians to mitigate complications and optimise outcomes. For more surgical and procedural prep content, visit our Clinical Skills Overview page.