Table of Contents
Overview – Thyroid Examination
A thyroid examination is a vital component of both general medical assessment and targeted endocrine evaluation. It plays a central role in diagnosing thyroid disorders such as Graves’ disease, Hashimoto’s thyroiditis, thyroid malignancies, and goitre-related complications. This OSCE skill tests a candidate’s ability to inspect, palpate, percuss, and auscultate the thyroid region while identifying systemic features of hypo- or hyperthyroidism and evaluating for red flags like malignancy, tracheal compression, and retrosternal extension.
This page outlines a comprehensive and high-yield thyroid examination for medical students preparing for OSCEs, including key signs, clinical reasoning tips, and associated pathologies.
Definition
The thyroid examination is a structured clinical skill used to evaluate the thyroid gland for signs of dysfunction, enlargement, nodules, or associated systemic features. It also includes signs of thyroid eye disease and relevant neurological, dermatological, and cardiovascular findings.
Preparation
- Wash hands and introduce yourself.
- Confirm patient’s name and age.
- Explain the procedure and obtain consent.
- Position the patient seated upright with neck exposed.
Inspection
General Inspection
- Look around the bed for medications (e.g. thyroxine, beta-blockers).
- Assess patient appearance:
- Body mass index (BMI)
- Appropriateness of clothing (e.g. light clothing in winter = hyperthyroidism)
- Agitation/restlessness → Hyperthyroidism
- Lethargy/hypoactivity → Hypothyroidism
- Hoarseness, stridor, or dyspnoea → Suggest retrosternal goitre or malignancy
Hands
Mnemonic: TTV SO PPP
- Thyroid acropachy / Clubbing – Graves’
- Temperature – Cold/dry in hypothyroid; hot in hyperthyroid
- Vitiligo – Suggests autoimmune cause (Hashimoto’s)
- Onycholysis (Plummer’s nails)
- Palmar erythema
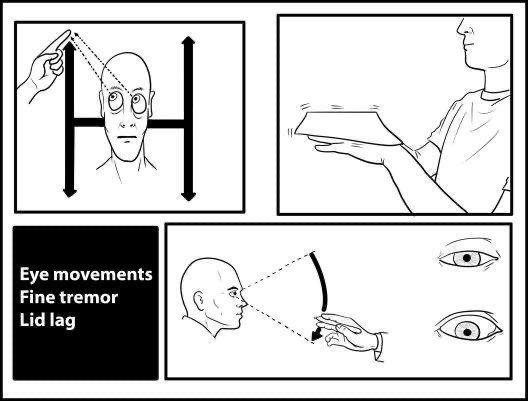
- Postural tremor – Fine tremor with paper test
- Pulse rate – Tachycardia/AF in hyperthyroidism, bradycardia in hypothyroidism
- Phalen’s and Tinel’s test – Carpal tunnel syndrome in hypothyroidism
Face
- Coarse hair, loss of lateral eyebrows, puffy face → Hypothyroidism
- Myxoedema (hypothyroid), round face
- Graves’ ophthalmopathy:
- Exophthalmos/Proptosis – Look from above
- Chemosis, conjunctivitis, corneal ulceration
- Ophthalmoplegia – Restricted eye movement (H test)
- Stellwag’s sign – Reduced blinking
- Lid lag test – Visible sclera on downward gaze
Neck Examination
Inspection
- Scars – Thyroidectomy (may be erythematous or faint)
- Midline swelling – Assess symmetry and number of nodules
- Prominent veins – Suggest thoracic inlet obstruction
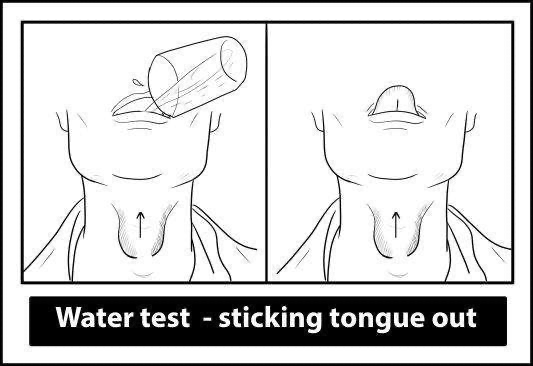
- Swallow test – Moves with swallowing = thyroid
- Tongue protrusion – Moves = thyroglossal cyst
Palpation
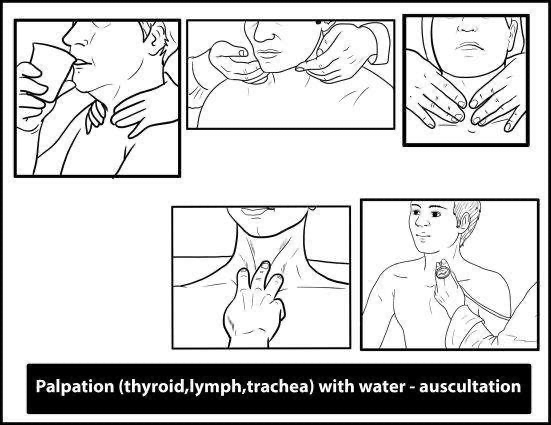
- Stand behind the patient; gently flex the neck forward
- Palpate each lobe and isthmus
- Assess for:
- Size, symmetry, tenderness
- Surface: smooth (Graves’), nodular (MNG), hard/fixed (malignancy)
- Retrosternal extension: feel for lower border, water swallow test
- Palpate lymph nodes (especially Delphian node)
Percussion
- Percuss the sternum – dullness suggests retrosternal extension
Auscultation
- Bruit over lobes – Suggests high vascularity (e.g. Graves’)
Neuromuscular and Systemic Features
- Proximal myopathy – Stand from a chair with arms crossed
- Reflexes – Slow relaxing (hypothyroid), brisk (hyperthyroid)
- Pretibial myxoedema – Graves’
- Non-pitting oedema – Hypothyroidism
- Pemberton’s sign – Facial congestion on arm elevation (retrosternal goitre)
- Kocher’s test – Tracheal compression
- Berry’s sign – Absent carotid pulse (malignancy)
- Cardiac – Listen for flow murmurs or signs of heart failure (e.g. crepitations)
- Scalp – Palpate for bony metastases (follicular carcinoma)

Assessment of Goitres and Nodules
Types of Goitre
- Diffuse goitre – Graves’ disease
- Multinodular goitre (MNG) – Toxic or non-toxic
- Solitary thyroid nodule (STN) – May be benign or malignant
Red Flags for Malignancy
- Male, age <20 or >70
- Single, firm, fixed nodule
- Rapid growth
- Voice changes (RLN palsy), dysphagia
- Cervical lymphadenopathy
- Family history, prior radiation exposure
Investigations
- Thyroid Function Tests – TSH, T3, T4
- Thyroid ultrasound:
- Malignant features: solid, hypoechoic, irregular borders
- Benign: cystic, hyperechoic, well-defined
- FNAC classification:
- Non-diagnostic
- Benign
- AUS/FLUS
- Follicular neoplasm
- Suspicious for malignancy
- Malignant
- Thyroid scan – Hot (benign), cold (malignant)
- CT/X-ray – Tracheal compression
- Laryngoscopy – Assess vocal cord function
- Tumour markers:
- Thyroglobulin – Papillary/follicular
- Calcitonin – Medullary
- RET proto-oncogene testing – MEN syndromes
Management
Medical
- Hyperthyroidism:
- Antithyroid drugs (carbimazole, PTU)
- Beta-blockers for symptoms
- Hypothyroidism:
- Levothyroxine replacement
Surgical
- Indications:
- Malignancy
- Large or retrosternal goitre
- Refractory hyperthyroidism
- Types of thyroidectomy:
- Lobectomy, subtotal, near-total, total
- Complications:
- Hypoparathyroidism (hypocalcaemia)
- Hypothyroidism
- RLN injury
- Tracheal injury, haematoma, infection
Radioiodine Therapy
- Especially for toxic nodules and Graves’
- Contraindicated in pregnancy, breastfeeding, young patients
Summary – Thyroid Examination
The thyroid examination is a core OSCE skill for identifying thyroid dysfunction and detecting potential red flags like malignancy or retrosternal extension. It requires careful inspection, palpation, and evaluation of systemic signs such as eye changes, tremors, reflexes, and neck masses. For a broader context, see our Clinical Skills Overview page.