Table of Contents
Overview – Venous Vascular Examination
The venous vascular examination is a core clinical skill used to assess for chronic venous insufficiency (CVI), deep vein thrombosis (DVT), and varicose veins. It is frequently examined in surgical OSCEs and is crucial for identifying vascular pathologies that may lead to complications like venous ulcers, thrombophlebitis, and pulmonary embolism. This examination includes detailed inspection, palpation, and special tests to assess vein valve competence and identify underlying pathology.
Definition
The venous vascular examination involves a clinical assessment of the lower limb venous system to evaluate for superficial or deep venous disease, valve incompetence, or thromboembolic phenomena.
Preparation
- Wash hands and introduce yourself.
- Confirm patient details and obtain consent.
- Expose both legs fully – shorts preferred.
- Patient should be standing, unless specific tests require lying down.
- Look around for walking aids, medication, and signs of comorbidity.
Inspection
- Inspect legs front, sides, and back, including between toes and soles.
- Signs of chronic venous insufficiency (progresses in stages):
- Telangiectasia, reticular veins
- Varicose veins
- Edema (loss of bony landmarks)
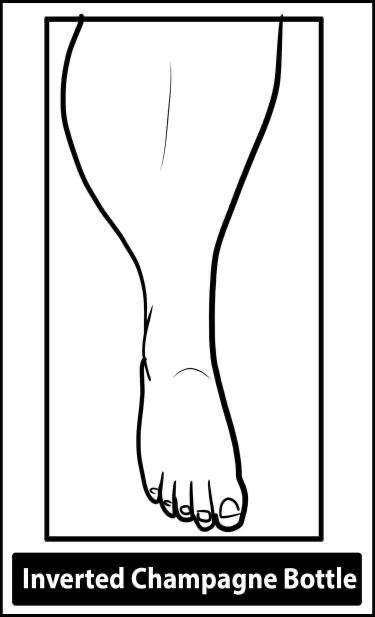
- Brown pigmentation (hemosiderin), eczema, lipodermatosclerosis (inverted champagne bottle appearance)
- Atrophie blanche
- Venous ulcers (medial gaiter area): assess size, site, border, base, discharge
- Additional findings:
- Erythema → DVT, thrombophlebitis
- Scars from prior vein surgery
- Ankle flares (dilated venules near the malleolus)
- Saphena varix (saphenofemoral junction bulge)
- DVT signs:
- Phlegmasia cerulea dolens – blue, swollen, painful leg
- Phlegmasia alba dolens – pale, pulseless, cold leg
Palpation
- Pitting edema – press over ankles/shins
- Tenderness:
- Calf – suspect DVT (use fingertips)
- Medial to femoral pulse – iliofemoral DVT
- Tender cords – thrombophlebitis (along great saphenous)
- Temperature:
- Use backs of hands to compare both legs
- Increased warmth may indicate DVT or cellulitis
Special Tests
1. Cough Impulse Test
- Place fingers over saphenofemoral junction (2.5 cm below and lateral to pubic tubercle)
- Ask patient to cough
- Impulse = positive for SFJ incompetence (varicose veins)
2. Schwartz (Tap) Test
- Patient standing
- Tap lower great saphenous vein and feel for impulse proximally
- Positive = superficial vein valve incompetence
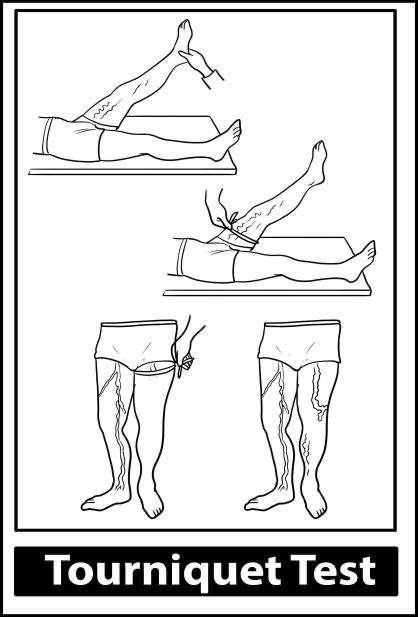
3. Trendelenburg (Tourniquet) Test
- Patient supine
- Elevate leg to 90°, empty veins
- Apply tourniquet at SFJ
- Ask patient to stand and observe:
- Rapid filling after tourniquet release = SFJ incompetence
- Filling during tourniquet = perforator vein incompetence
4. Perthes Test
- Apply tourniquet at SFJ
- Ask patient to walk
- Pain or engorgement of superficial veins = deep vein obstruction
5. Homan’s Sign
- Passive dorsiflexion of foot → calf pain suggests DVT (low sensitivity/specificity)
6. Auscultation
- Listen over large varicosities
- Bruit suggests arteriovenous (AV) fistula
Venous Anatomy Overview
Superficial Veins
- Great saphenous vein (GSV): medial ankle to groin (SFJ)
- Short saphenous vein (SSV): lateral ankle to popliteal fossa
Deep Veins
- Accompany arteries (e.g. femoral, popliteal)
Perforator Veins
- Connect superficial to deep system
- Named perforators:
- Cockett (medial ankle)
- Boyd (knee)
- Dodd (distal thigh)
- Hunterian (mid-thigh)
Differential Diagnosis of Leg Swelling
- Varicose veins
- DVT
- Chronic venous insufficiency
- Lymphoedema
- Baker’s cyst
- Lipodermatosclerosis
- Arterial insufficiency (if pulses absent)
- Pelvic/abdominal mass compressing veins (e.g. tumour, pregnancy)
CEAP Classification (for CVI)
- C – Clinical class (e.g. C0–C6: telangiectasia → ulceration)
- E – Etiology (primary, secondary, congenital)
- A – Anatomy (superficial, deep, perforator)
- P – Pathophysiology (reflux, obstruction)
Investigations
- Duplex Ultrasound – confirms venous reflux or DVT
- D-dimer – supports DVT suspicion
- Wells Score – pre-test probability for DVT
- Contrast venography or MR venography – complex cases
- Rule out pelvic/abdominal masses with abdominal exam or imaging
Management
Varicose Veins
- Conservative:
- Compression stockings
- Leg elevation
- Interventional:
- Sclerotherapy (telangiectasia/reticular veins <4 mm)
- Endovenous laser ablation (EVLA) or radiofrequency ablation (VNUS)
- Subfascial endoscopic perforator surgery (SEPS) for perforator incompetence
- Stripping or Trendelenburg procedure for SFJ incompetence
Venous Ulcers
- Dressing
- Compression (Unna boot)
DVT
- Anticoagulation with LMWH and warfarin
Complications
- Saphenous nerve injury (GSV stripping)
- Sural nerve injury (SSV procedures)
- Hematoma
- Infection
- DVT/PE
- Recurrent varicosities
Summary – Venous Vascular Examination
The venous vascular examination is essential for identifying chronic venous insufficiency, DVT, and varicose veins. It incorporates key OSCE techniques including inspection for ulcers and pigmentation, palpation for edema and tenderness, and special tests like Trendelenburg and Perthes to assess valve function. For a broader context, see our Clinical Skills Overview page.