Table of Contents
Overview – Acute Hypertension
Acute hypertension refers to a sudden, severe elevation in blood pressure that may present with or without target organ damage. While most chronic hypertension is asymptomatic, acute hypertensive episodes—especially hypertensive crises—can be life-threatening. Early recognition and careful blood pressure control are essential to reduce the risk of cerebral, cardiac, and renal complications.
Aetiology
Primary (Essential) Hypertension – ~95%
- Idiopathic origin; likely multifactorial and not curable
- Risk factors:
- Family history, age
- High-salt and high-cholesterol diet
- Obesity, diabetes mellitus
- Smoking and alcohol use
- Stress
Subtypes
- Isolated Diastolic Hypertension
- More common in older men
- Isolated Systolic Hypertension
- In young adults: Often due to increased sympathetic drive and elevated cardiac output
- In older adults: Due to decreased arterial compliance (e.g. fibrosis, calcification)
Secondary Hypertension – ~5%
- Cardiovascular: Coarctation of the aorta, hypervolaemia, rigid vessels
- Renal:
- Acute glomerulonephritis
- Chronic kidney disease
- Polycystic kidney disease
- Renal artery stenosis
- Endocrine:
- Hyperadrenalism (e.g. Cushing’s syndrome)
- Acromegaly
- Thyroid dysfunction
- Phaeochromocytoma
- Neurological:
- Raised intracranial pressure
- Psychogenic causes
- Sleep apnoea
- Acute stress
- Pregnancy-related:
- Pre-eclampsia: Placental ischaemia triggers release of vasoactive mediators → maternal hypertension as compensation
Hypertensive Crisis (Malignant Hypertension)
Definition
A hypertensive crisis is a medical emergency characterised by severely elevated blood pressure (>200/120 mmHg) accompanied by signs of end-organ damage.
End-Organ Manifestations
- Retinopathy:
- Papilloedema
- Flame haemorrhages
- Optic disc swelling
- Brain:
- Hypertensive encephalopathy
- Mental status changes
- Risk of stroke or cerebral oedema
- Kidneys:
- Acute kidney injury (elevated creatinine)
- Heart:
- Pulmonary oedema
- Congestive heart failure
Common Triggers
- Abrupt withdrawal of antihypertensive therapy
- Sympathetic overactivity
- Drug use (e.g. cocaine, amphetamines)
- Glomerulonephritis
- Head trauma
- Tumours (e.g. phaeochromocytoma)
- Pre-eclampsia
Pathophysiology
- Thought to involve failure of vascular autoregulation
- Sudden spike in systemic vascular resistance
- Vicious cycle of escalating vascular damage, ischaemia, and organ dysfunction
Symptoms
- Severe headache
- Confusion or drowsiness
- Visual disturbances (e.g. blurred vision due to papilloedema)
- Nausea and vomiting
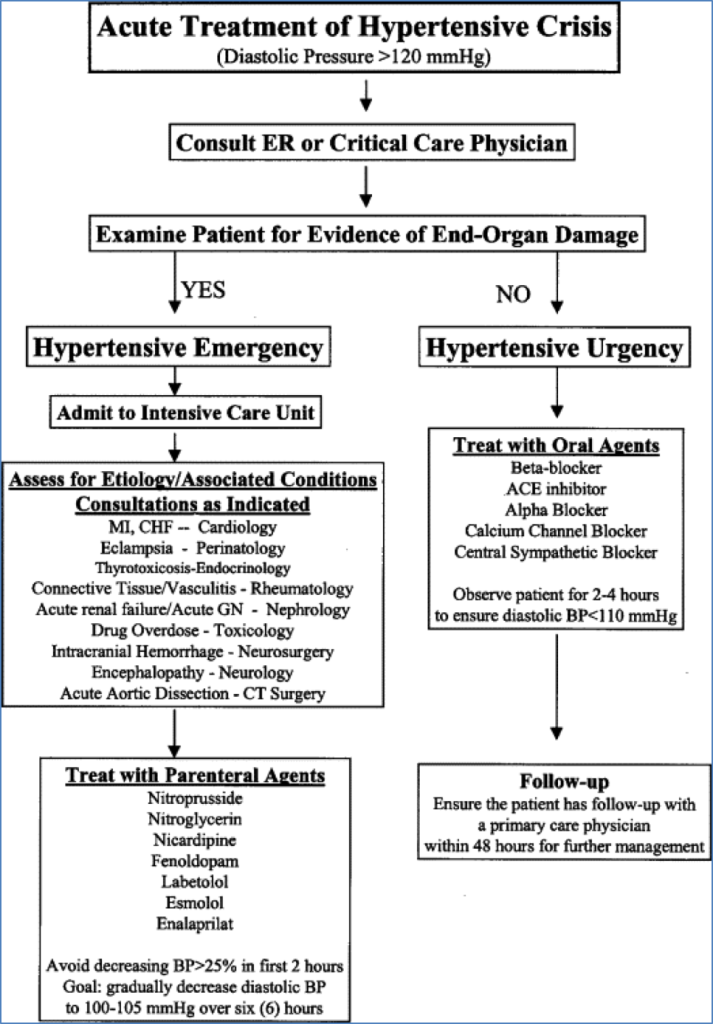
Management
- Goal: Gradual reduction of BP to ~150/90 mmHg over 24–36 hours
- Rapid BP drops can precipitate ischaemia in coronary, cerebral, or renal circulations
- Management must be guided by local protocols and the presence of end-organ damage
Disclaimer: Always refer to local or hospital-specific guidelines when managing hypertensive crises.
Summary – Acute Hypertension
Acute hypertension may be due to primary or secondary causes and can escalate into a hypertensive crisis with rapid-onset vascular damage. Recognising high-risk features such as altered mental status, retinopathy, and renal dysfunction is essential. Management focuses on controlled blood pressure reduction to prevent organ ischaemia. For a broader context, see our Emergency Medicine Overview page.