Table of Contents
Overview – Chest X-Ray Interpretation
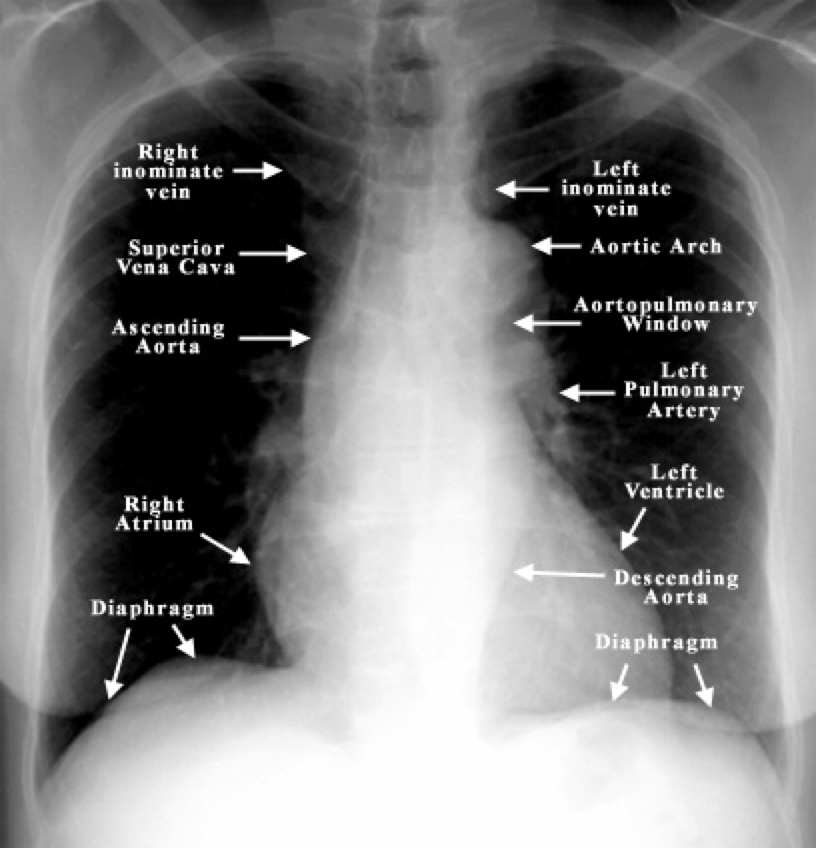
Chest X-ray interpretation is an essential clinical skill in emergency medicine. It allows rapid, bedside evaluation of critical thoracic pathology including pneumothorax, pleural effusion, pulmonary oedema, infection, and cardiomegaly. This guide outlines a systematic approach for final-year medical students, covering technical adequacy, anatomical structures, and red flag findings.
Definition
Chest X-ray (CXR) interpretation involves a systematic analysis of thoracic anatomy using radiographic imaging. It assists in diagnosing acute and chronic conditions affecting the lungs, heart, mediastinum, bones, and soft tissue.
Aetiology (Clinical Context of Use)
CXRs are used to evaluate patients presenting with:
- Chest pain
- Dyspnoea
- Cough and fever
- Trauma
- Suspected pulmonary or cardiac disease
Technical Considerations
1. Confirm Patient and Image Details
- Correct patient name, date, and orientation
2. Determine Projection Type
- PA (Posteroanterior):
- Standard view, beam travels back → front
- Heart is near plate → minimal magnification
- Reliable for assessing cardiomegaly
- AP (Anteroposterior):
- Portable films or ICU patients
- Heart is further from plate → may appear artificially enlarged
- Supine:
- Patient lying flat
- Common in trauma/critical care
- Erect:
- Upright film (standing/sitting)
- Lateral:
- Side-on view for localisation or behind-heart lesions
- Mobile:
- Bedside; usually AP and supine
3. Technical Adequacy
- Inspiration:
- ≥8 posterior ribs should be visible above diaphragm
- Penetration:
- Adequate = vertebral bodies just visible behind heart
- Overpenetrated → overly black lungs
- Underpenetrated → white lungs
- Rotation:
- Medial ends of clavicles equidistant from spinous processes

Systematic Review of the CXR
4. Structures to Review
- Heart:
- Normal size = <50% chest width (PA view)
- Cardiomegaly may indicate heart failure, LV/RV hypertrophy, or pericardial effusion
- Mediastinum:
- Evaluate borders of aorta, heart, diaphragm
- Trachea:
- Should be midline
- Deviation may suggest tension pneumothorax, collapse, or large effusion
- Carina:
- Bifurcation of bronchi
- Widened/distorted → consider malignancy
- Lungs:
- Uniform markings; extra markings = increased density
- Causes: oedema, infection, fibrosis, malignancy
- Diaphragm:
- Right dome higher (due to liver)
- Blunted costophrenic angles = pleural effusion
- Bones & Soft Tissues:
- Check ribs, clavicles, spine
- Assess for fractures or soft tissue swelling
Areas Easily Missed
- Lung apices (look for TB, pneumothorax)
- Hilar regions (lymphadenopathy, vessel dilation)
- Behind the heart (posterior lesions)
- Costophrenic angles (effusions)
Key Radiological Findings
Trachea
- Midline = normal
- Deviation = possible tension pneumothorax, large effusion, or lung collapse (opposite side)
Carina
- Angle may widen/distort in mediastinal lymphadenopathy (e.g. malignancy)
Bronchi
- Right bronchus is more vertical and shorter → more likely site of aspiration
Costophrenic Angles
- Sharp = normal
- Blunted/obscured = pleural effusion
- Look for meniscus sign
Lung Markings
- Should taper towards periphery
- Extra markings: fibrosis, oedema, infection, tumour
- Pneumonia:
- Consolidation; patchy or lobar opacification
- Pulmonary Oedema:
- Kerley B lines (horizontal lines at lung bases)
Hilar Region
- Should be symmetrical
- Enlargement = dilated vessels or lymphadenopathy
Heart Borders
- Well defined margins
- May be obscured by adjacent pathology (e.g. pneumonia)
Cardiothoracic Ratio
- Heart width >50% chest width = cardiomegaly
Summary – Chest X-Ray Interpretation
Chest X-ray interpretation is a foundational diagnostic skill for evaluating acute thoracic presentations. A structured approach—starting from projection type and technical adequacy, through to anatomical review—enables accurate recognition of key findings like pneumonia, pleural effusion, pulmonary oedema, and cardiomegaly. For a broader context, see our Emergency Medicine Overview page.