Table of Contents
Overview – Diabetic Emergencies
Diabetic emergencies are acute, life-threatening complications of diabetes mellitus, including diabetic ketoacidosis (DKA), hyperosmolar non-ketotic coma (HONC), and hypoglycaemia. Prompt recognition and treatment are essential to prevent organ dysfunction, neurological injury, or death. This page outlines the causes, diagnosis, and management of these emergencies, integrating pathophysiology and clinical reasoning for high-stakes scenarios.
Definition
Diabetic emergencies refer to critical presentations of dysregulated blood glucose due to insulin deficiency, resistance, or treatment imbalance. They include:
- Diabetic Ketoacidosis (DKA)
- Hyperosmolar Non-Ketotic Coma (HONC)
- Hypoglycaemia
Diagnostic Criteria – Diabetes Overview
Diagnostic “7–11 Rule”
- Fasting BSL ≥ 7.0 mmol/L
- Random BSL > 11.0 mmol/L
- OGTT (2-hour post-load) > 11.0 mmol/L
Other Diagnostic Considerations
- Type 1 Diabetes Markers
- Anti-Islet-Cell Antibodies (Anti-ICA)
- Anti-GAD (Glutamic Acid Decarboxylase) Antibodies
- HbA1c used for monitoring, not diagnosis
- Impaired Glucose Tolerance: Elevated BSLs not high enough for diabetes diagnosis
Clinical Features – Initial Presentation
- Classic triad: Polyuria, Polydipsia, Polyphagia (PPP)
- Unexplained weight loss, fatigue, lethargy
- Recurrent infections, delayed healing, e.g. genital candidiasis
Diabetic Ketoacidosis (DKA)
Aetiology
- Typically in Type 1 Diabetes
- Often due to missed insulin or intercurrent illness
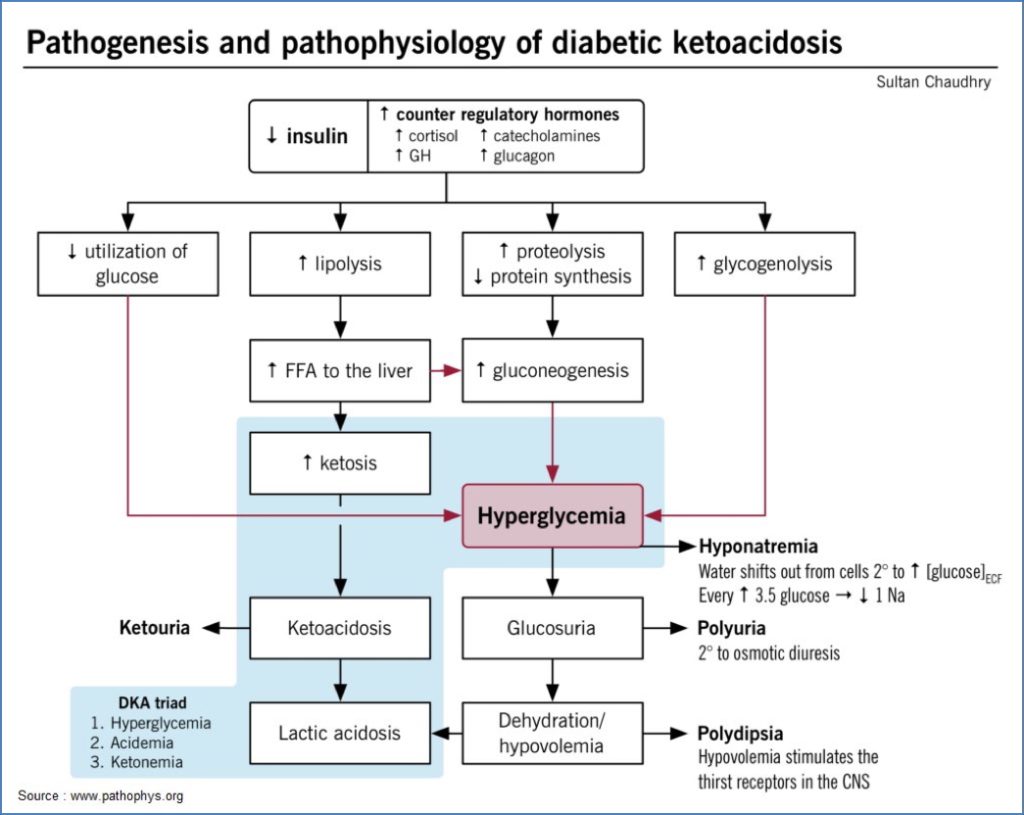
Pathophysiology
- Insulin deficiency → Glucose uptake failure
- ↑ Counter-regulatory hormones → Lipolysis → Ketogenesis
- Hyperglycaemia → Osmotic diuresis → Dehydration
Diagnosis
- BGL > 15 mmol/L
- Ketonuria
- Metabolic acidosis: pH ↓, HCO₃⁻ < 15 mmol/L
- Sweet/acetone breath
Symptoms
- Polyuria, polydipsia, weight loss
- Vomiting, dehydration
- Hyperventilation (Kussmaul breathing), acetone breath
- Electrolyte abnormalities (↓ Na⁺, ↓ K⁺) → Arrhythmias
Treatment
- IV Fluids – for dehydration
- IV Insulin Infusion – to reduce glucose
- Monitor and Replace Electrolytes – especially potassium
Complications
- Up to 40% mortality if untreated
- Severe dehydration, electrolyte collapse
Hyperosmolar Non-Ketotic Coma (HONC)
Aetiology
- Typically in Type 2 Diabetes
- Relative insulin deficiency + stress/illness
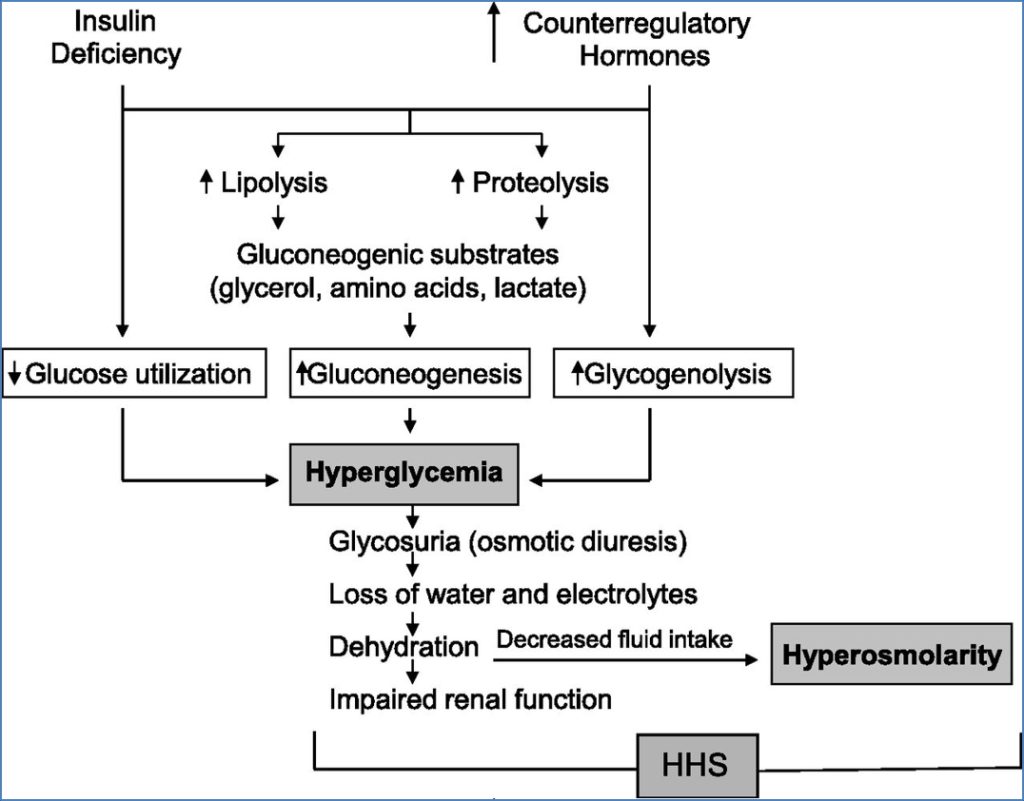
Pathophysiology
- Enough insulin to suppress ketogenesis
- Not enough to prevent severe hyperglycaemia
- Result: profound dehydration and hyperosmolarity without ketosis
Diagnosis
- Hyperglycaemia (often very high)
- Osmolality > 330 mOsm/kg
- No ketones or acidosis
Symptoms
- Confusion, coma
- Polyuria, severe dehydration
- Neurological signs: seizures, tremors, hyporeflexia
Treatment
- IV Fluids
- IV Insulin + K⁺ supplementation
- Electrolyte correction
Complications
- Often fatal if untreated
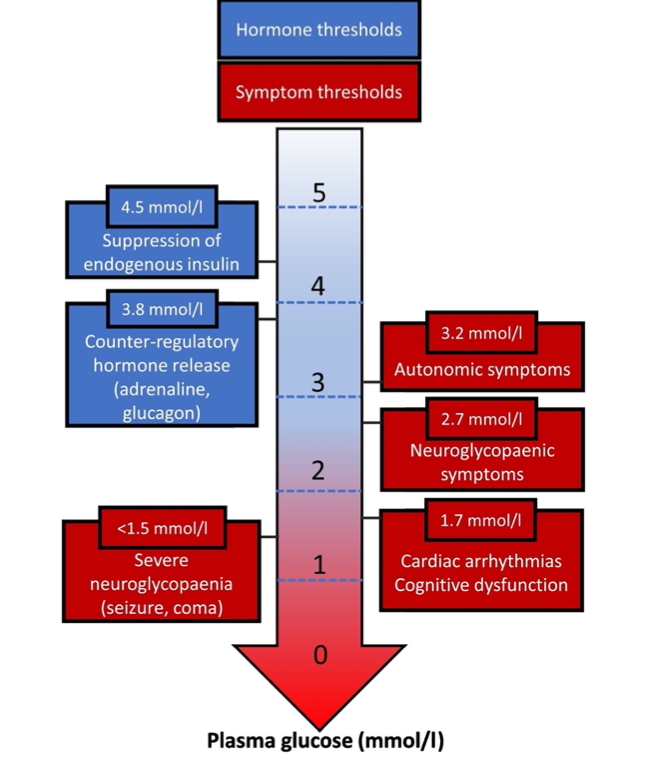
Hypoglycaemia
Definition
- BSL < 6.0 mmol/L
- Severe: BSL < 3.5 mmol/L
Aetiology
- Diabetes + Insulin overdose
- Alcohol, exercise, missed meals
- Sepsis
Symptoms
Neurogenic (Adrenergic)
- Palpitations, anxiety, tremor
Neurogenic (Cholinergic)
- Hunger, sweating, paraesthesia
Neuroglycopaenic
- Behaviour change, confusion
- Seizures, coma
Summary:
- Autonomic: Tremor, dizziness, sweating, anxiety
- CNS: Confusion, drowsiness, visual changes
Treatment
- Mild: Oral glucose (e.g. jellybeans, juice)
- Severe: IV dextrose or IM/IV glucagon
- Always: ABC support
Summary – Diabetic Emergencies
Diabetic emergencies such as DKA, HONC, and hypoglycaemia are critical presentations requiring prompt diagnosis and treatment. Understanding their underlying mechanisms, clinical features, and management strategies is vital for patient survival. For a broader context, see our Emergency Medicine Overview page.