Table of Contents
Overview – Loss of Consciousness
Loss of consciousness (LOC), or altered level of consciousness (ALOC), is a common emergency presentation with a wide differential diagnosis ranging from head trauma and drug overdose to metabolic derangement and infection. Recognising and managing the underlying cause early is vital to prevent secondary brain injury and improve outcomes. This article outlines key causes, assessment tools like the Glasgow Coma Scale, and a structured approach to managing LOC.
Causes of Loss of Consciousness
Head Trauma
- Primary brain injury (determines best possible outcome):
- Concussion
- Cerebral contusion
- Laceration
- Diffuse axonal injury
- Secondary brain injury (determines actual outcome):
- Hypoxia
- Hypoglycaemia
- Reduced cerebral perfusion (hypotension, haemorrhage, oedema)
- Goal of treatment: Prevent secondary injury
Drugs
- Prescription Medications:
- Accidental overdose (especially in elderly or suicide risk)
- Drug interactions: analgesics, sedatives, antidepressants
- Recreational Drugs:
- Alcohol
- Opiates and others
- Management:
- Treat specific overdose
- Assess for suicidality
- Consider psychiatric review
Tumours
- Rare cause of acute LOC
- May be benign or malignant
- Can be primary or metastatic
Systemic Causes
- Hypoxia
- Hypoventilation
- Hypotension
- Sepsis
Endocrine Causes
- Diabetes:
- Hypoglycaemia
- Hyperglycaemia or diabetic ketoacidosis (DKA)
- Always check blood glucose, even if other causes seem obvious (e.g. trauma, stroke)
- Thyroid dysfunction:
- Hypothyroidism
- Thyrotoxicosis
Metabolic Causes
- Uraemia: Due to acute or chronic kidney failure
- Hepatic failure: Often from alcoholic liver disease
Infection
- Meningitis (diagnosis is critical)
- Encephalitis
- Tuberculosis
- Malaria
Assessment of ALOC
Glasgow Coma Scale (GCS)
- Max Score = 15: Awake, alert, responsive
- GCS <10: Deeply unconscious
- GCS <8: Coma → May require intubation
- Min Score = 3: Deep coma or death

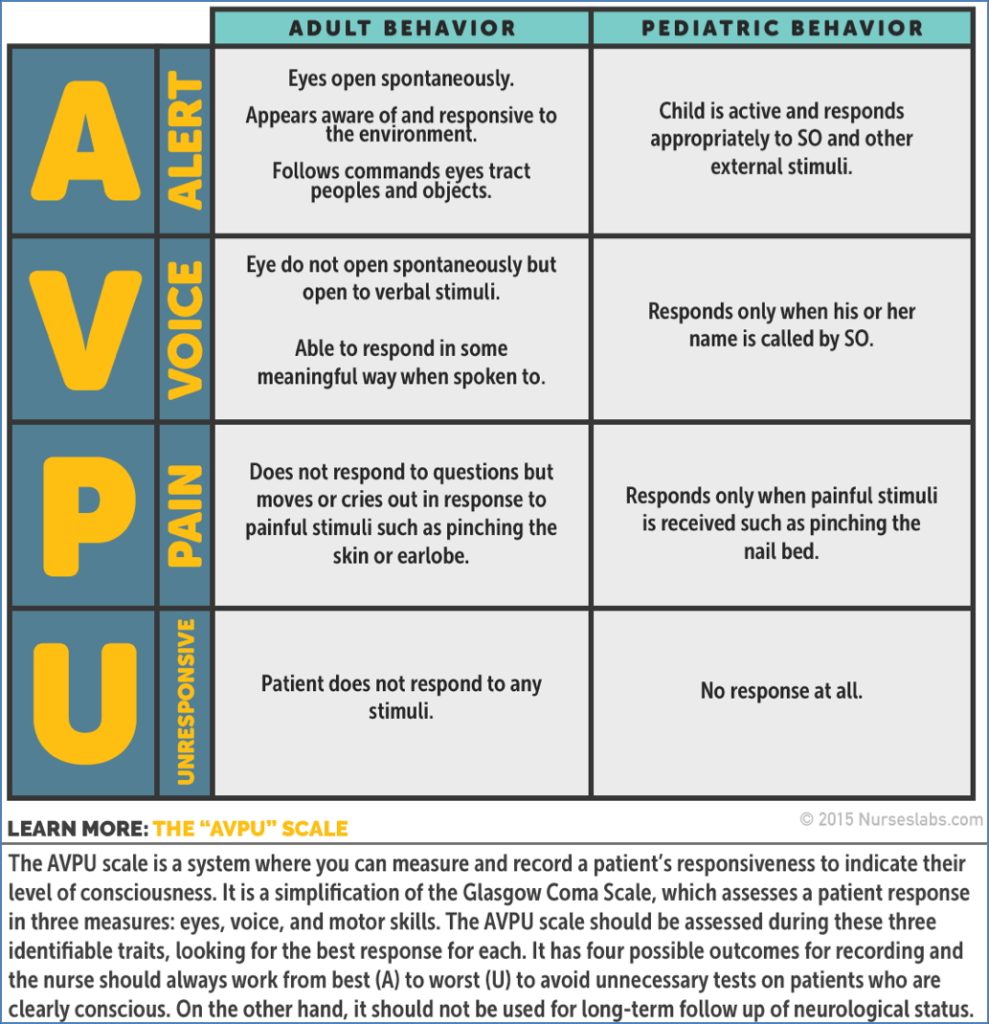
AVPU Scale
- Simple alternative to GCS:
- Alert
- Responds to Verbal stimuli
- Responds to Pain
- Unresponsive
Traumatic Brain Injury Severity (TBI)
- Mild: GCS 14–15 → 10% positive CT, 1% need neurosurgery
- Moderate: GCS 9–13 → 40% positive CT, 8% need neurosurgery
- Severe: GCS <9 → ~40% mortality
Practice Cases – AVPU & GCS (for clinical learning)
Case 1:
- 16 y/o female fell from third floor balcony, groans, withdraws from pain
- AVPU: P
- GCS: 8 (E1, V2, M5)
Case 2:
- 24 y/o male, intoxicated, slurred speech, disoriented but cooperative
- AVPU: A
- GCS: 14 (E4, V4, M6)
Case 3:
- 82 y/o febrile woman, confused, aggressive verbal response
- AVPU: A
- GCS: 13 (E4, V4, M5)
Case 4:
- 6-month-old post-seizure, eyes open, no response
- AVPU: U
- GCS: Difficult to apply accurately in infants
- Note: GCS and AVPU have limited use in infants due to developmental variation—use paediatric-specific tools
Management Framework for ALOC
Primary Survey: ABCDEFG
A – Airway
- Most common cause of LOC = airway obstruction
- Clear airway using:
- Left lateral position
- Suction
- Guedel airway
- Jaw thrust
- GCS <8 → Intubate
B – Breathing
- Ensure oxygenation
- Prevent secondary brain injury from hypoxia
- Maintain normocarbia
- Hypoventilation → Hypercarbia → Vasodilation → ↑ICP → ↓Cerebral perfusion
C – Circulation
- Ensure adequate perfusion
- Give IV fluids as needed
- Cerebral Perfusion Pressure = MAP – ICP
- In TBI, even 5 minutes of hypotension increases mortality by 25%
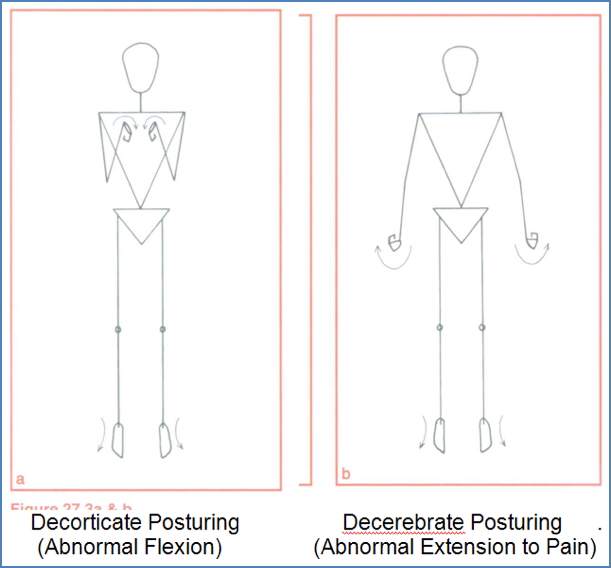
D – Disability
- Assess and monitor level of consciousness
- Check pupils (size/reactivity)
- Document changes
E – Exposure
- Examine entire body
- Don’t forget to check the back
F – Fingerstick
- Always check blood glucose regardless of suspected cause
G – Glucose
- Hypoglycaemia is a reversible and common cause of LOC
History
- Past medical history
- Medications or drug use
- Collateral history (from family, witnesses)
- Recent trauma?
- Overseas travel?
Examination
- Repeat primary survey
- Look for trauma, needle marks
- Signs of infection: fever, neck stiffness, focal neurology
- Observe respiratory effort
Investigations
- Full blood count (FBC)
- Biochemistry and glucose
- Urea & electrolytes
- Blood cultures (if infection suspected)
- Lumbar puncture (for CSF)
- Head CT or MRI
Specific Treatment
- Cause-specific treatment where possible
- Naloxone for opioid overdose
- Insulin or glucose for diabetic emergencies
- Supportive care always includes:
- Oxygen
- IV fluids
- Glucose
- Empirical antibiotics if infection suspected
Summary – Loss of Consciousness
Loss of consciousness (LOC) or altered level of consciousness (ALOC) has a broad differential ranging from trauma and overdose to infection and metabolic causes. A structured approach using ABCDE, GCS/AVPU, and targeted investigations is key to early intervention and prevention of secondary brain injury. For a broader context, see our Emergency Medicine Overview page.