Table of Contents
Overview – Medical Emergency Framework
The medical emergency framework is a structured approach used by healthcare professionals to assess and manage critically unwell patients. It ensures timely triage, life-saving interventions, effective pain control, and identification of reversible causes in life-threatening scenarios. Mastery of this framework is essential for final-year medical students preparing for real-world emergency presentations.
Definition
- Emergency: A medical condition requiring immediate treatment (not always life-threatening).
- Triage: The process of sorting patients based on urgency of care needs.
- Resuscitation: Reviving someone from unconsciousness or apparent death.
- Primary Survey (ABCDE):
- Airway
- Breathing
- Circulation
- Disability
- Expose
- Retrieval Medicine: Pre-hospital emergency care via ambulance, helicopter, etc.
- National Triage Scale: Localized, standard triage guidelines (may differ by region and specialty).
Emergency Assessment Framework
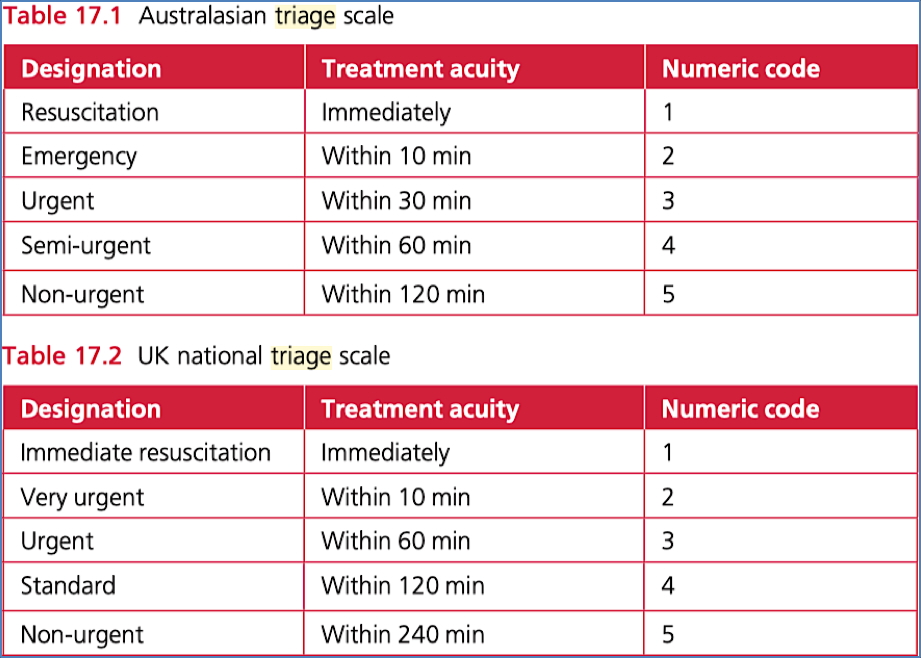
1. Triage
- Performed by specially trained emergency department (ED) nurses.
- Establishes priority of care using standardized scales.
- Asks: “This patient should wait for medical assessment no longer than ___ minutes?”
- Scales vary by region (e.g., Australian and UK triage systems).
- Children and psychiatric patients may require separate triage tools.
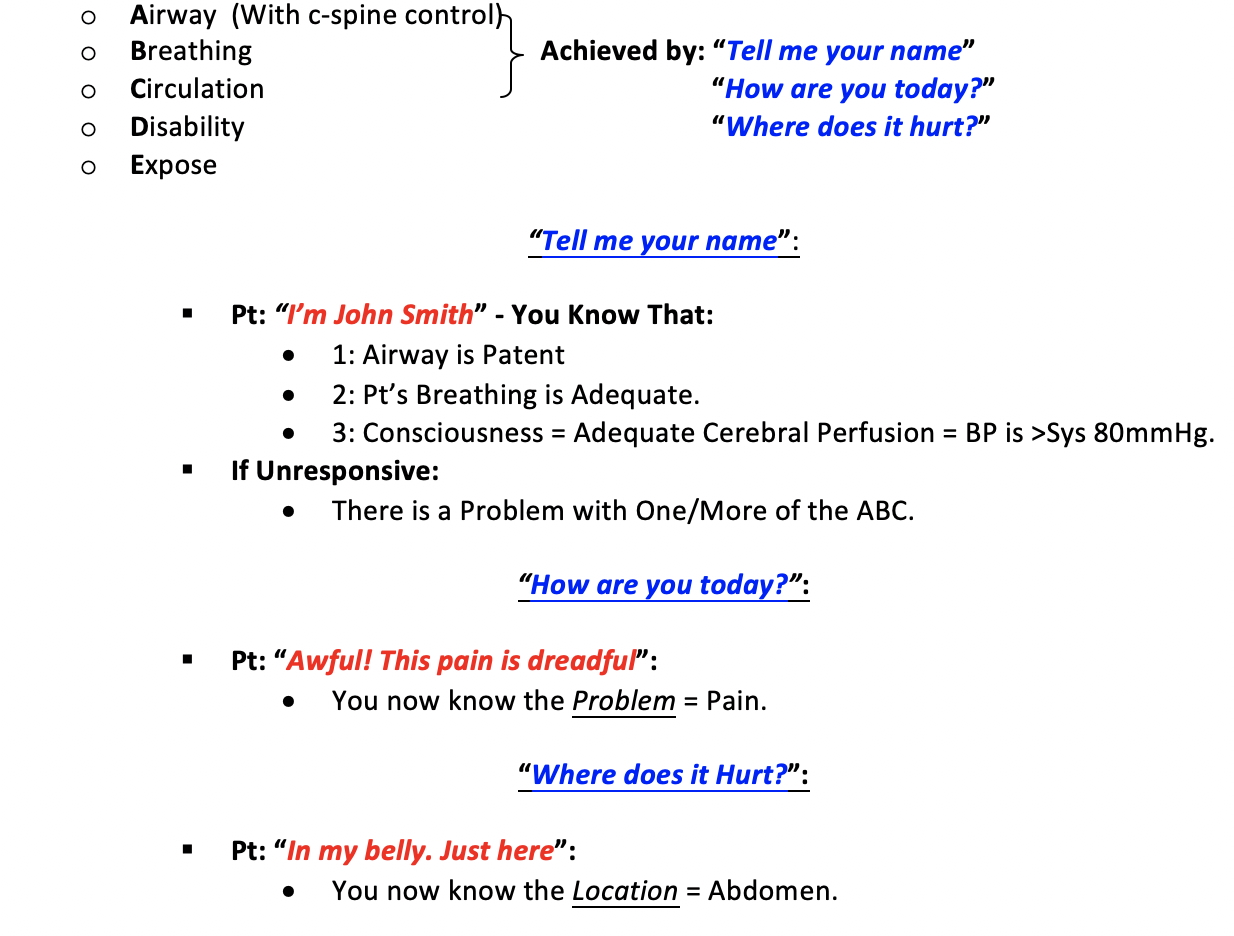
2. 30-Second Primary Survey (ABCDE)
Airway (with C-spine control)
- Assess ability to speak: e.g. “Tell me your name”
- If able to respond → airway patent, breathing adequate, and BP likely >80 mmHg systolic
- If unresponsive → immediate airway/breathing/circulation issue
Breathing
- Observe for visible chest rise, respiratory effort
- Ask: “How are you today?” → Helps assess oxygenation and respiratory status
Circulation
- Ask: “Where does it hurt?” → Identify location and assess perfusion
- Simultaneously check:
- Pulse – rate, rhythm, volume
- Skin – temperature, sweating
- Colour – cyanosis, jaundice, pallor
- Neck – JVP, thyroid, trauma
You now have an approximation of:
- Respiratory rate
- Pulse (e.g. tachycardic, bradycardic, bounding)
- Skin temperature (e.g. hot, cold)
- Oxygen saturation (e.g. presence of cyanosis)
Disability
- Assess mental status, pain, and neurological response
Exposure
- Visual inspection of chest, abdomen, limbs
- Full exposure while preserving dignity and temperature

3. Pain Assessment
After stabilizing ABCs, pain assessment is the next priority
Pain Features:
- Site – Localisation and radiation
- Onset – Sudden vs gradual, with or without trauma
- Character – Sharp, dull, burning, etc.
- Intensity – At rest and with movement
- Duration – Continuous or intermittent
- Aggravating factors
Somatic vs Visceral Pain:
- Somatic – Sharp, localised, tender
- Visceral – Dull, poorly localised, with referred symptoms
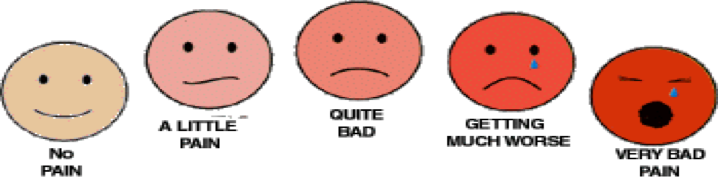
Pain Scales:
- Categorical – Mild/Moderate/Severe
- Numeric – 0 to 10
- Visual Analogue – Emoticon-based (useful for deaf, foreign, or paediatric patients)
Importance of Early Analgesia:
- Reduces pain and anxiety
- Improves cooperation and communication
- May reduce physiological symptoms (e.g. tachycardia)
Common Analgesic Options:
- Oral (e.g. Paracetamol) – Cheap, but limited potency
- Parenteral (e.g. IM/IV opioids) – Effective, but complex
- Regional nerve blocks – Best for isolated injuries
4. Mnemonic: AMPLE
Useful for gathering emergency history:
- Allergies
- Medications
- Past medical history
- Last meal
- Events leading to presentation
5. Early Management Goals
- Prevent complications: Intervene early to limit organ/system damage
- Minimise suffering: Timely, accurate care reduces distress and enhances outcomes
Basic Life Support
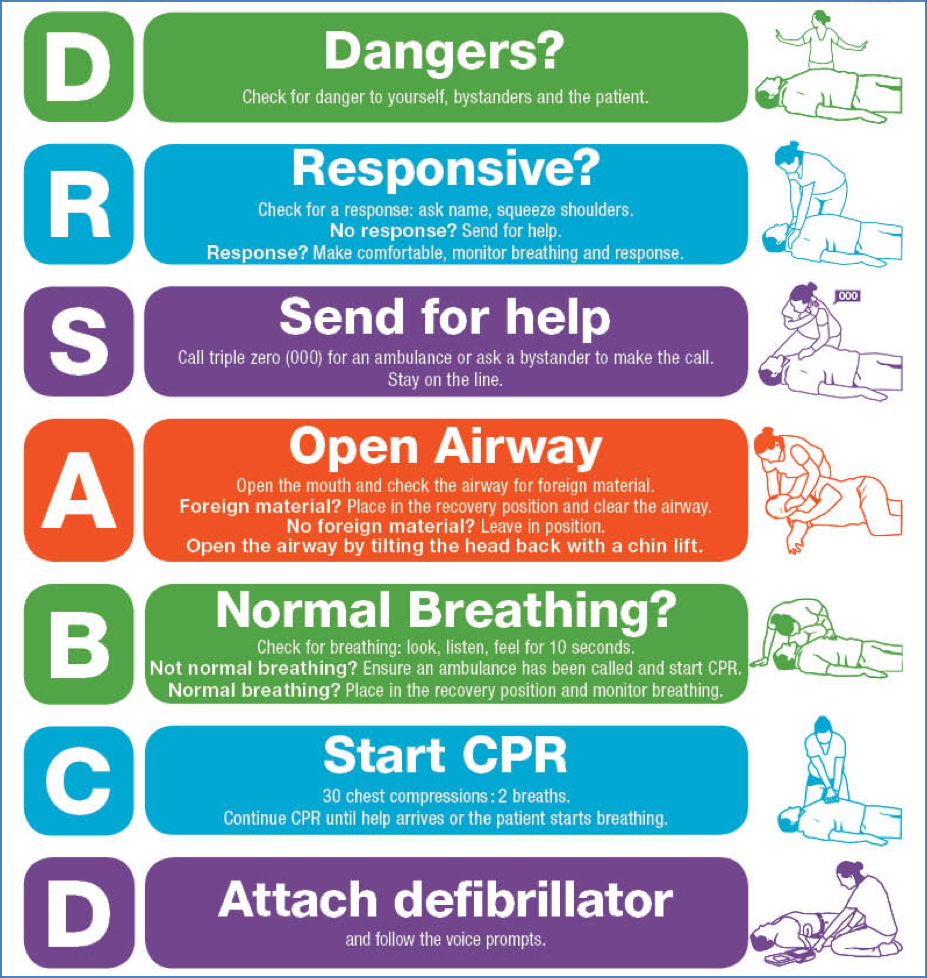
Disclaimer: Follow your local/hospital guidelines
Initial resuscitation in unresponsive patients includes basic airway support, chest compressions, and calling for help (resuscitation team).
Advanced Life Support
Disclaimer: Follow your local/hospital guidelines
Key Priorities:
- Lay patient flat
- Precordial thump (only within seconds of arrest if no defibrillator present)
- Head tilt–chin lift
- Begin CPR if unresponsive and not breathing
- Call resuscitation team
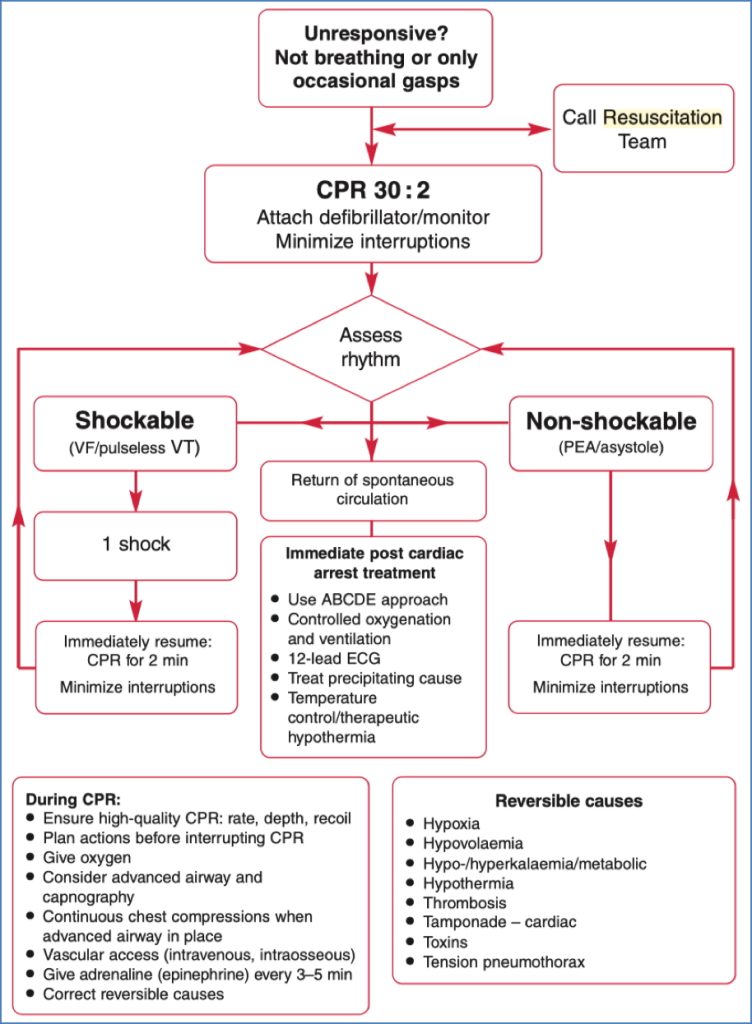
Potentially Reversible Causes of Cardiac Arrest (4 H’s & 4 T’s)
The 4 H’s
- Hypoxia:
- Ensure O2 at 15 L/min
- Check tidal volume and chest movement
- Hypovolaemia:
- Causes: Trauma, GI bleed, ruptured AAA, ectopic pregnancy
- Give stat fluids, identify source, alert surgical teams
- Hypo/Hyperkalaemia & Metabolic causes:
- Check electrolytes
- Treat with calcium chloride (10 mL of 10%) or K+ bolus (5 mmol IV) as needed
- Hypothermia:
- Core rewarming for severe hypothermia (<30°C)
- Consider pleural/peritoneal lavage or extracorporeal methods
The 4 T’s
- Thrombosis (e.g. PE):
- Consider fluid bolus, CPR, and thrombolysis
- Tamponade:
- Clinical signs: Hypotension, JVP rise, muffled heart sounds
- Emergency pericardiocentesis
- Toxins:
- Consider based on history (e.g. TCA overdose)
- Treat with antidotes or supportive care
- Tension Pneumothorax:
- Rapid needle decompression → chest drain
Post-Resuscitation Care
- Continue CPR until pulse and signs of life return
- Maintain SpO₂ between 94–98%
- Check ABGs (PaCO₂ 35–45 mmHg)
- Insert gastric tube
- Contact cardiology if suspected acute coronary syndrome
- Treat seizures (e.g. midazolam, lorazepam, diazepam)
- Maintain blood glucose (6–10 mmol/L)
- Transfer to ICU or cardiac unit
Summary – Medical Emergency Framework
The medical emergency framework outlines a structured, life-saving approach to critically unwell patients, incorporating triage, ABCDE survey, pain control, and advanced life support. Recognising reversible causes and delivering early management is crucial for improving outcomes. For a broader context, see our Emergency Medicine Overview page.