Table of Contents
Overview – Fluid Balance
Fluid balance is essential for maintaining normal cellular function, chemical homeostasis, excitable tissue activity, and blood pressure regulation. Through a tightly controlled interplay of intake and output, the body preserves extracellular and intracellular fluid volumes, mediated primarily by hormonal and neural feedback mechanisms. Understanding fluid balance is crucial for managing numerous clinical conditions, including dehydration, shock, and electrolyte disturbances.
Definition
- Fluid balance refers to the regulation of body water volume and its distribution across compartments.
- Electrolyte balance (particularly sodium and potassium) is closely linked, especially for excitable tissues such as nerves and muscles.
- It is vital for:
- Cell function.
- Chemical stability of extracellular fluids.
- Blood pressure homeostasis.
Body Fluid Compartments
- Total fluid volume: ~40 liters in an adult.
- Extracellular fluid (ECF): 15 liters
- Plasma: 3 liters.
- Interstitial fluid: 12 liters.
- Intracellular fluid (ICF): 25 liters
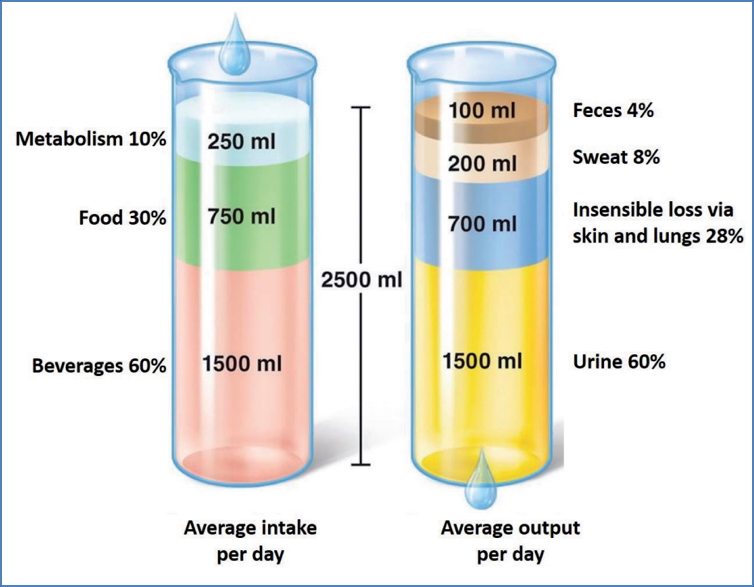
Water Intake & Output
Intake
- Metabolic production (~250 mL).
- Food (~750 mL).
- Beverages (~1500 mL).
- Total: ~2500 mL/day.
Output
- Faeces (~100 mL).
- Sweat (~200 mL).
- Insensible loss via lungs and skin (~700 mL).
- Urine (~1500 mL).
Regulation of Water Intake (Thirst Mechanism)
- Controlled by the hypothalamus and triggered by:
- Decreased plasma volume (>10% loss):
- ↓ Salivary gland blood flow → dry mouth → stimulates thirst centre.
- Increased plasma osmolality (1–2% rise):
- Osmoreceptor dehydration in hypothalamus → thirst stimulation.
- Decreased plasma volume (>10% loss):
- Hypovolemia also activates baroreceptors, which stimulate thirst and renin release from the kidneys.
Regulation of Water Output
Obligatory Water Loss
- Unavoidable fluid loss via:
- Faeces, sweat, lungs, and minimum urine output (~500 mL).
Regulated Water Loss
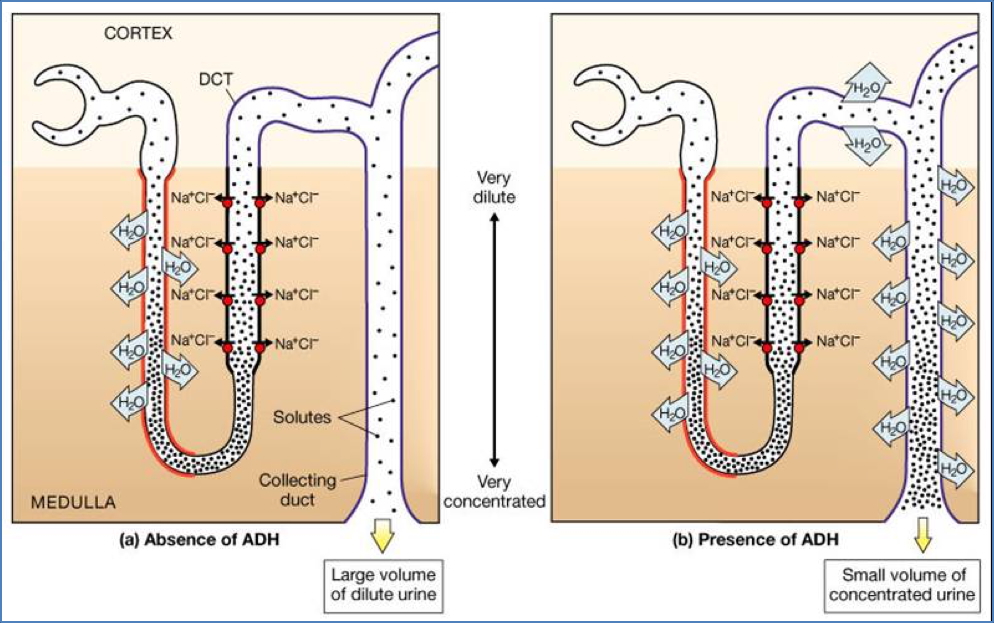
- Controlled primarily by Antidiuretic Hormone (ADH).
Antidiuretic Hormone (ADH)
- Secreted by: Posterior pituitary.
- Stimulated by:
- ↑ Plasma osmolality (via osmoreceptors).
- ↓ Plasma volume.
- Mechanism:
- Normally, distal tubules and collecting ducts are impermeable to water.
- ADH increases aquaporin channels → ↑ water permeability → water reabsorption.
- Promotes water conservation and increases blood volume.

2. https://www.austincc.edu/apreview/PhysText/Renal.html
Atrial Natriuretic Peptide (ANP)
- Secreted by: Atrial myocytes.
- Stimulated by: Atrial stretch from elevated blood volume/pressure.
- Actions:
- Dilates afferent and constricts efferent arterioles → ↑ glomerular filtration.
- Inhibits:
- Renin secretion → suppresses renin-angiotensin system.
- Aldosterone release.
- ADH release.
- Promotes sodium and water excretion → ↓ blood volume and pressure.
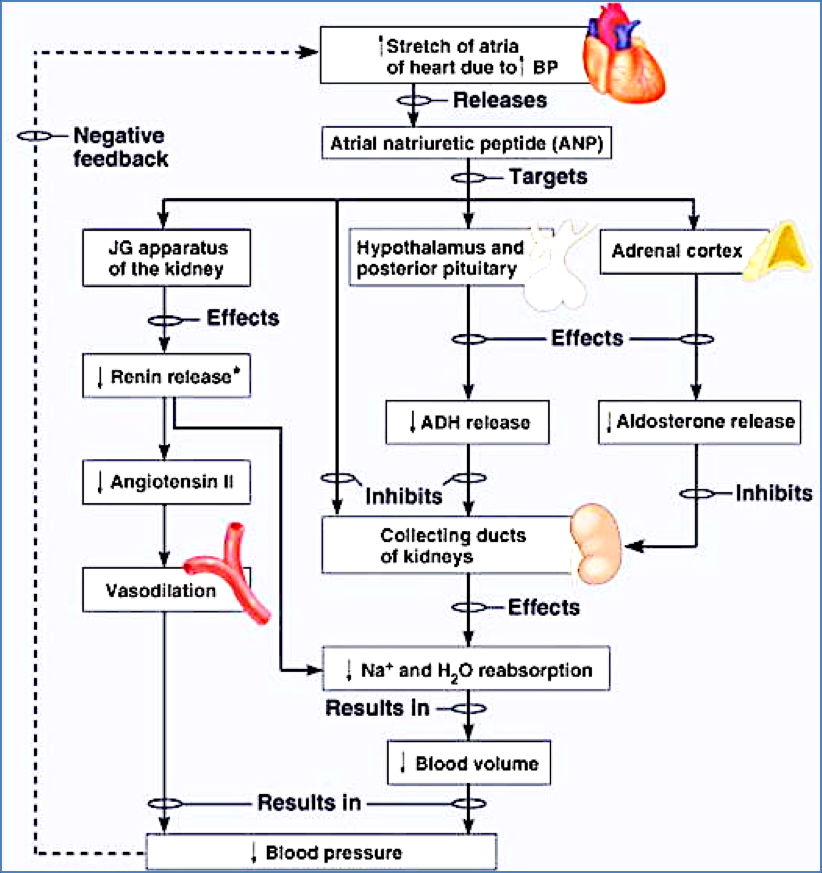
Summary – Fluid Balance
Fluid balance is maintained through the coordinated regulation of intake and output by the hypothalamus, kidneys, and cardiovascular system, with key hormonal influences from ADH and ANP. These systems work together to preserve stable fluid compartments, osmotic balance, and blood pressure. For a broader context, see our Endocrine Overview page.