Table of Contents
Overview – Hyperparathyroidism
Hyperparathyroidism is a condition characterised by inappropriate overproduction of parathyroid hormone (PTH), resulting in disturbances in calcium and phosphate metabolism. It is typically classified as either primary (autonomous overproduction of PTH, often due to adenoma) or secondary (compensatory increase in PTH due to chronic hypocalcaemia, commonly from renal failure). The condition can lead to serious skeletal, gastrointestinal, neurological, renal, and cardiovascular complications, and should be promptly recognised and managed.
Definition
- Hyperparathyroidism refers to ↑ PTH secretion, which leads to:
- ↑ Osteoclastic bone resorption → hypercalcaemia
- ↑ Renal phosphate excretion → hypophosphataemia
Types
Primary Hyperparathyroidism
- Cause: Autonomous overproduction of PTH
- Aetiologies:
- Parathyroid adenoma (most common; sporadic or MEN syndromes)
- Parathyroid hyperplasia
- Parathyroid carcinoma
Clinical Features
- Female > Male
- Classic triad of symptoms:
- “Bones, Moans & Abdominal Groans”:
- Bone: Pain, osteoporosis, pathological fractures
- Moans: Depression, lethargy, seizures
- Abdominal Groans: Constipation, peptic ulcers, gallstones
- Additional signs:
- Renal: Nephrolithiasis (kidney stones)
- Cardiovascular: Aortic/mitral valve calcifications
- “Bones, Moans & Abdominal Groans”:
Diagnosis
- ↑ PTH
- ↑ Serum calcium
- ↓ Serum phosphate
Management
- Surgical excision of the affected parathyroid gland(s)
Secondary Hyperparathyroidism
- Cause: Reactive ↑ PTH secretion in response to chronic hypocalcaemia
- Aetiology:
- Chronic renal failure (most common)
- Vitamin D deficiency
- Dietary calcium deficiency
Pathogenesis
- Renal failure → phosphate retention and ↓ vitamin D activation → ↓ serum calcium
- Hypocalcaemia → stimulates compensatory ↑ PTH secretion → parathyroid hyperplasia
Clinical Features
- Symptoms of chronic kidney disease
- Bone-related symptoms (osteopenia/osteoporosis)
Management
- Vitamin D supplementation
- Oral calcium
- Partial parathyroidectomy (in refractory cases)
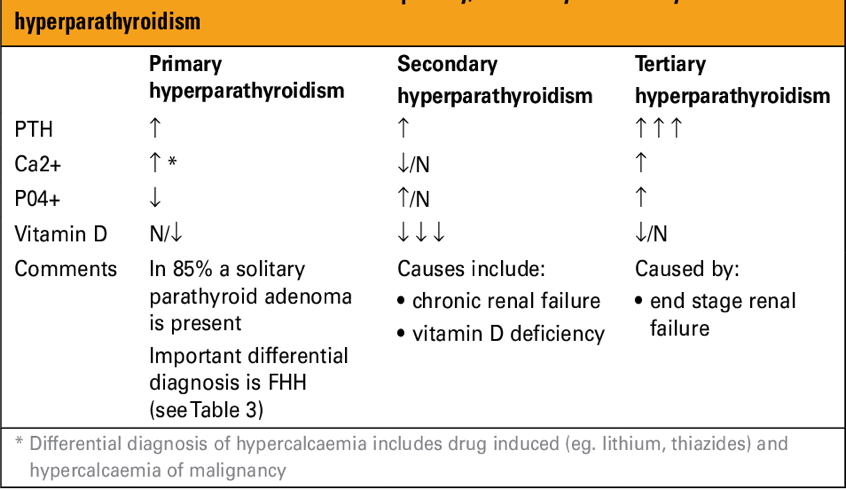
Summary – Hyperparathyroidism
Hyperparathyroidism is characterised by excess secretion of PTH, leading to calcium and phosphate imbalances. Primary forms often result from adenomas and are symptomatic of hypercalcaemia, while secondary forms are typically due to chronic renal failure. Prompt recognition and treatment—ranging from surgical excision to medical management—are essential to prevent end-organ complications. For more, visit the Endocrine Overview page.