Table of Contents
Overview – Reproductive Endocrinology
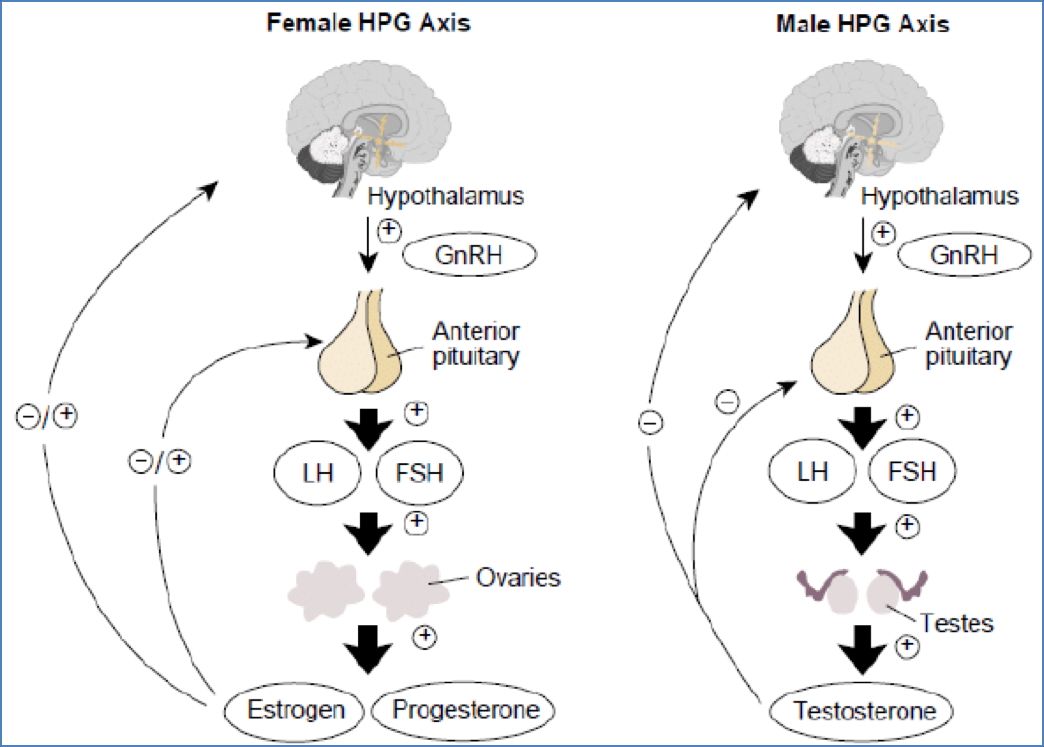
Reproductive endocrinology governs human fertility and sexual development through the tightly regulated hypothalamic-pituitary-gonadal axis. The interplay of gonadotropins and sex steroids controls gametogenesis, secondary sexual characteristics, menstrual cycling, and pregnancy maintenance, making this system clinically important for both male and female reproductive health.
Definition
- Reproductive endocrinology refers to hormonal regulation of sexual development, gamete production, and reproductive function.
- Controlled primarily by:
- Hypothalamic gonadotropin-releasing hormone (GnRH).
- Pituitary gonadotropins (LH and FSH).
- Gonadal sex hormones (androgens, estrogens, and progesterone).
Hypothalamic-Pituitary-Gonadal (HPG) Axis
Hypothalamic Hormone
- Gonadotropin-Releasing Hormone (GnRH):
- Peptide hormone released in pulsatile fashion every ~90 minutes.
- Stimulates anterior pituitary release of FSH and LH.
Pituitary Hormones
- Follicle-Stimulating Hormone (FSH) and Luteinizing Hormone (LH):
- Glycoproteins secreted in response to GnRH pulsatility.
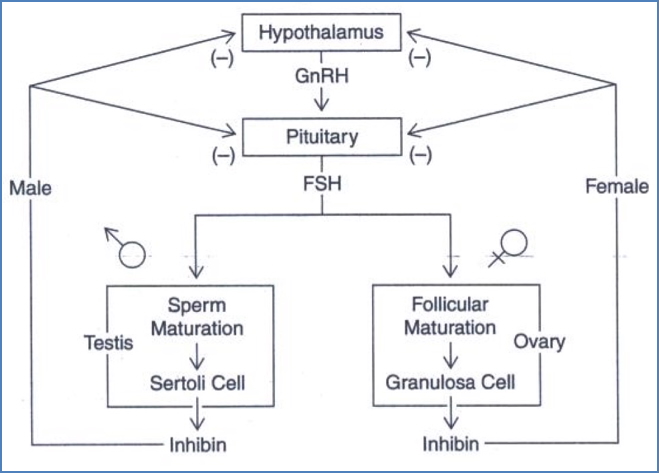
- Inhibin:
- Secreted by Sertoli cells (males) and granulosa cells (females).
- Provides negative feedback, selectively inhibiting FSH secretion.
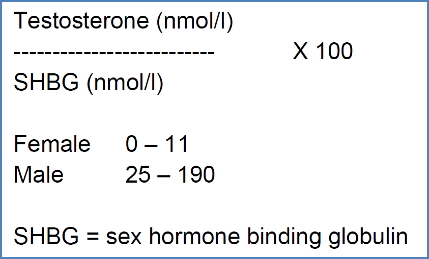
Sex Hormone Binding Globulin (SHBG)
- Transport protein produced by the liver.
- Increases with estrogen; decreases with androgens.
- Maintains stable levels in males; fluctuates in females, especially during pregnancy.
Androgens (Primarily Male Hormones)
- Testosterone (main androgen):
- 40% bound to SHBG, 60% to albumin, 2% free (biologically active).
- Intracellular receptors mediate its effects.
- Dehydroepiandrosterone (DHEA-S) and Androstenedione: peripheral androgen precursors.

Actions of Androgens
- Primary Sex Characteristics:
- Development and maintenance of reproductive tract.
- Libido and spermatogenesis enhancement.
- Secondary Sex Characteristics:
- Body hair, deepening of voice, bone growth, increased musculature, skin thickening, and androgen-binding protein synthesis.
Free Androgen Index
- Clinically used to estimate bioavailable testosterone fraction.
Estrogens and Progesterone (Primarily Female Hormones)
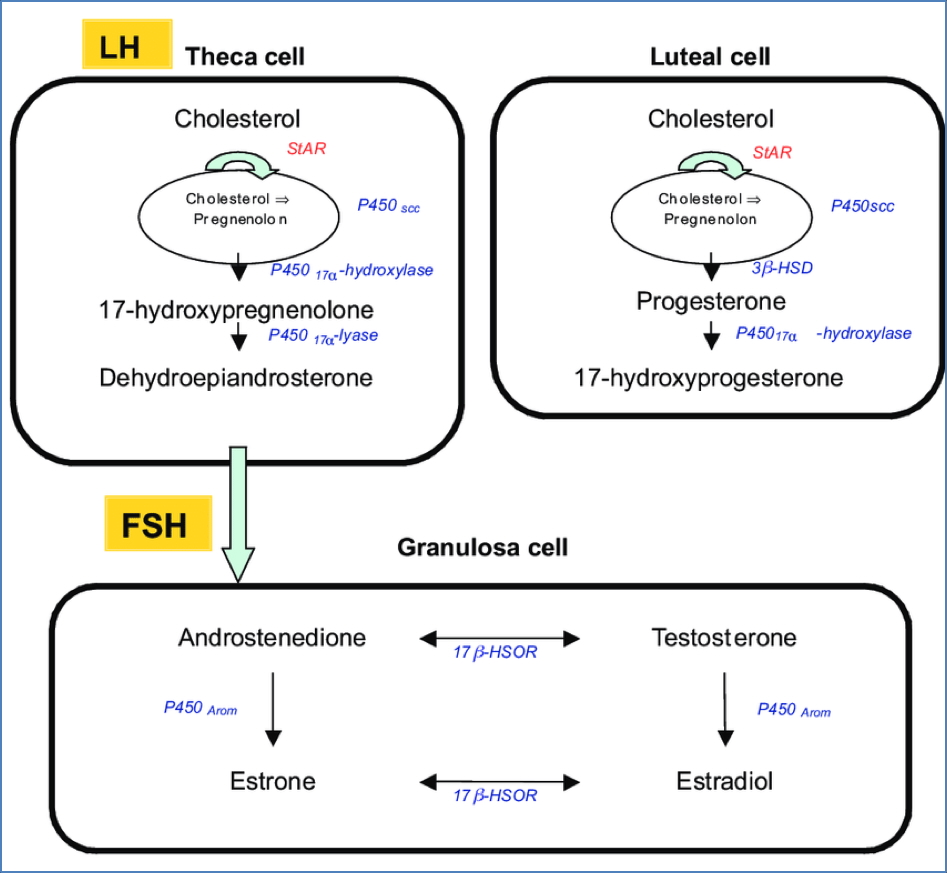
Estrogens
- Three forms: estradiol, estrone, estriol.
- Synthesized mainly by ovaries (corpus luteum), but also adrenal cortex, adipose tissue, and placenta.
- Derived from cholesterol via theca and granulosa cell cooperation (two-cell model).
Progesterone
- Secreted primarily by corpus luteum.
- Also synthesized from cholesterol.
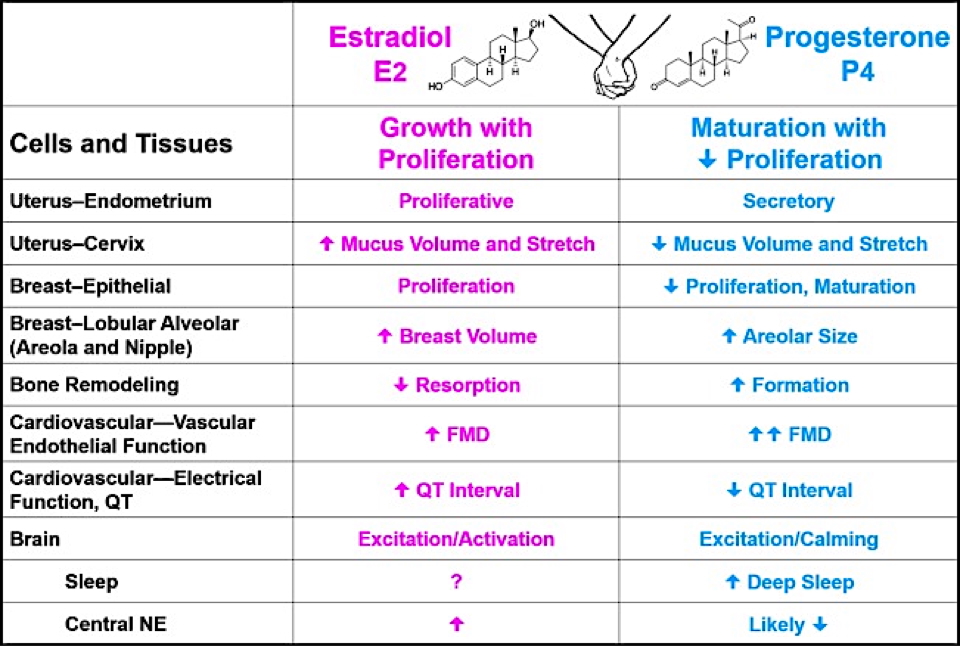
Actions of Estrogen
- Puberty:
- Development of reproductive organs and secondary sex characteristics.
- Menstruation:
- Endometrial proliferation pre-ovulation.
- Initiates LH surge for ovulation.
- Pregnancy:
- Supports myometrium, cervical ripening, mammary duct growth.
- Systemic:
- Bone anabolism, vascular flexibility, fat deposition.
Actions of Progesterone
- Menstruation:
- Dominant during luteal phase.
- Pregnancy:
- Maintains uterine quiescence, thickens cervical mucus, promotes glandular breast growth, raises basal respiratory rate.
- Systemic:
- Bone density promotion, skin elasticity.
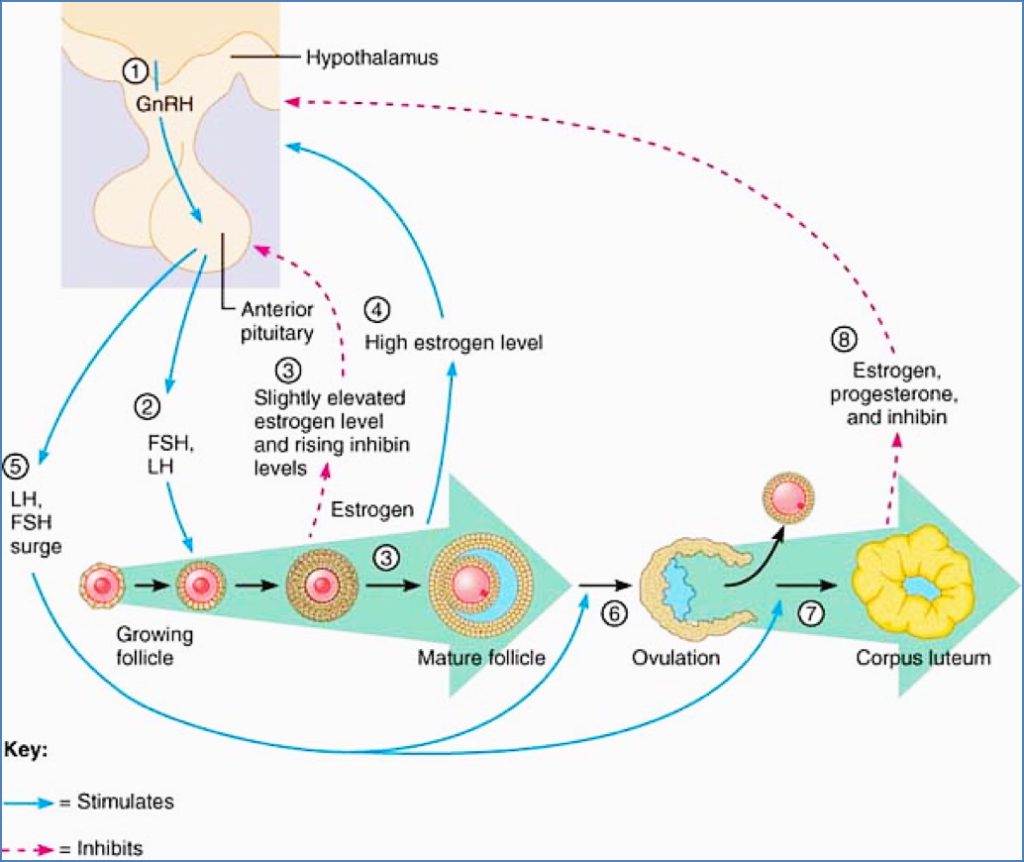
Regulation of the Ovarian Cycle
- GnRH pulses stimulate FSH and LH release.
- FSH drives follicle maturation; LH stimulates androgen production in theca cells.
- Androgens converted to estrogens by granulosa cells.
- Moderate estrogen → negative feedback; high estrogen → positive feedback (LH surge).
- LH surge triggers ovulation and corpus luteum formation.
- Corpus luteum secretes estrogen, progesterone, and inhibin → suppresses GnRH, FSH, LH.
- Corpus luteum regression leads to cycle renewal.
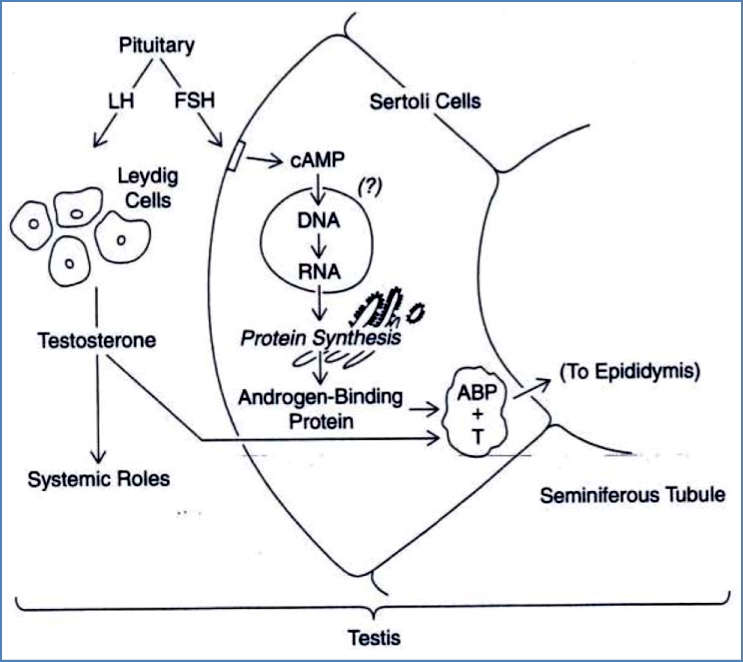
Regulation of Spermatogenesis
- GnRH stimulates FSH and LH release.
- FSH activates Sertoli cells to produce androgen-binding protein (ABP).
- LH activates Leydig cells to secrete testosterone.
- Testosterone + ABP → support spermatogenesis.
- Inhibin and testosterone provide negative feedback to GnRH.
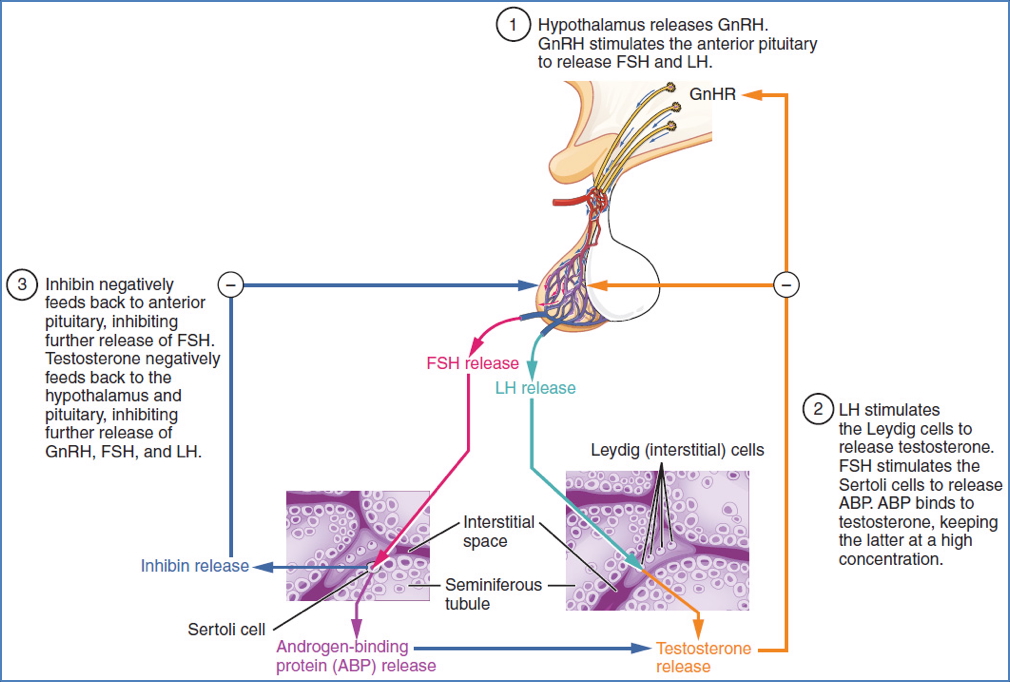
Sertoli Cell Functions
- Androgen binding protein production.
- Inhibin secretion.
- Blood-testes barrier maintenance.
- Spermatid nourishment and phagocytosis.
- Tubular fluid production.
- Plasminogen activator synthesis for sperm release.
Leydig Cell Functions
- Testosterone production under LH stimulation.
Summary – Reproductive Endocrinology
Reproductive endocrinology coordinates hormonal control of gametogenesis, menstrual cycling, and sexual maturation through the hypothalamic-pituitary-gonadal axis. Disruptions in this tightly regulated system underlie many reproductive disorders. For a broader context, see our Endocrine Overview page.