Table of Contents
Overview – Hypothyroidism
Hypothyroidism refers to the under-secretion of thyroid hormone, resulting in a broad range of systemic effects due to reduced metabolic activity. It is one of the most common endocrine disorders worldwide, with iodine deficiency and autoimmune Hashimoto’s thyroiditis being leading causes. Early recognition and management are crucial to prevent complications such as myxoedema coma and cretinism.
Definition
- Hypothyroidism: insufficient production or action of thyroid hormones (T3, T4).
- Leads to decreased metabolic rate and multi-system dysfunction.
Aetiology
Dietary Causes
- Iodine deficiency (most common worldwide cause, particularly in low-resource regions).
Autoimmune Causes
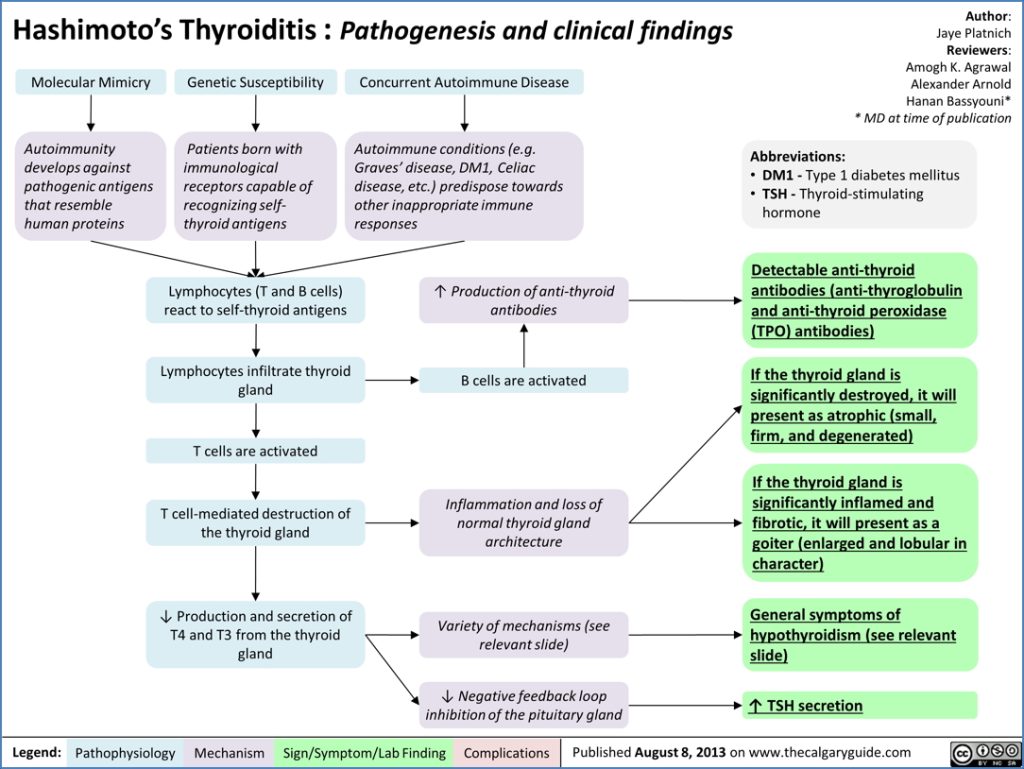
- Hashimoto’s thyroiditis (most common cause in developed countries):
- Autoantibodies:
- Anti-thyroid peroxidase (Anti-TPO Abs).
- Anti-thyroglobulin antibodies.
- Predominantly affects women >60 years.
- Autoantibodies:
Central Causes (Secondary Hypothyroidism)
- Hypothalamic-pituitary disorders:
- Decreased TRH or TSH secretion due to pituitary or hypothalamic failure.
Pathophysiology
- ↓ T3/T4 → ↓ Basal Metabolic Rate.
- ↓ Thermogenesis → Cold intolerance.
- ↓ Sympathetic sensitivity.
- Severe congenital hypothyroidism → Cretinism.
Clinical Features
General
- Fatigue
- Cold intolerance
- Apathetic facial expression
- Hoarseness
- Menstrual irregularities
- Muscle weakness
Cardiovascular
- Bradycardia
- Pericardial effusion
- Reduced cardiac output
Gastrointestinal
- Weight gain despite poor appetite
- Constipation
Neurological
- Paraesthesia
- Slow speech
- Mental sluggishness
Skin
- Pale, cool, dry skin
- Non-pitting oedema (face and periorbital) due to hyaluronic acid and glycosaminoglycan accumulation
Hair
- Dry, coarse hair
- Loss of lateral third of eyebrows
Musculoskeletal
- Muscle cramps
- Delayed relaxation of deep tendon reflexes (“hung reflexes”)
Haematological
- Macrocytic anaemia
Investigations
- TSH levels: elevated in primary hypothyroidism; low or normal in secondary causes.
- T4/T3 levels: low.
- Autoimmune screening (Hashimoto’s):
- Anti-thyroid peroxidase antibodies (Anti-TPO).
- Anti-thyroglobulin antibodies.
Management
First-line Treatment
- Thyroid hormone replacement:
- L-thyroxine (levothyroxine, T4).
- Preferred due to long half-life and peripheral conversion to active T3.
Complications
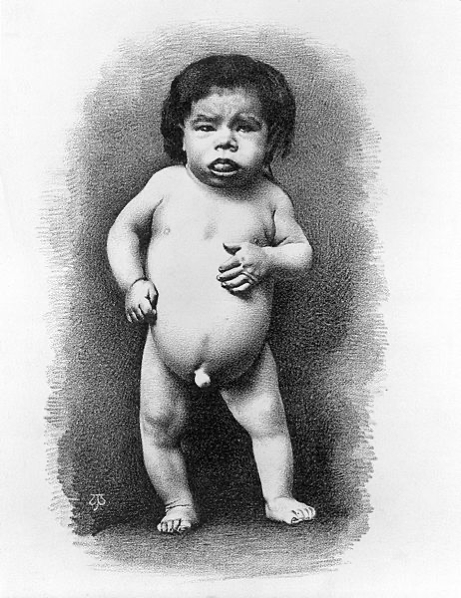
Cretinism
- Severe congenital hypothyroidism.
- Typically due to maternal iodine deficiency.
Clinical Features:
- Short stature
- Severe intellectual disability
- Coarse facial features
- Protruding tongue
- Umbilical hernia
Myxoedema Coma (Medical Emergency)
- Precipitated by infection, MI, CHF, or surgery in undiagnosed longstanding hypothyroidism.
Clinical Features:
- Hypothermia
- Hypoventilation
- Bradycardia
- Hypotension
- Hypoglycaemia
- Stupor or coma
Laboratory Findings:
- Severely low T3/T4
- Elevated TSH
- Hypoglycaemia
- Check ACTH and cortisol for possible adrenal insufficiency
Management:
- ABC stabilization
- Warming
- Loading dose IV thyroxine
- Hydrocortisone
- Assisted ventilation if necessary
- IV frusemide for pulmonary oedema
- Identify and treat precipitating cause
Summary – Hypothyroidism
Hypothyroidism is a common endocrine disorder characterized by under-secretion of thyroid hormones, leading to metabolic slowing and multi-organ involvement. Early diagnosis and appropriate thyroid hormone replacement prevent life-threatening complications such as cretinism and myxoedema coma. For a broader context, see our Endocrine Overview page.