Table of Contents
Overview – Thyroid Neoplasms
Thyroid neoplasms include both benign and malignant nodular growths of the thyroid gland. While most thyroid nodules are benign, it is important to evaluate them thoroughly to identify malignancy early. Hot nodules (autonomously functioning) tend to be benign, whereas cold nodules (hypofunctioning) raise concern for malignancy. Clinical assessment, imaging, and fine needle aspiration are central to diagnosis. This article explores the various types of thyroid neoplasms including adenomas and carcinomas.
Definition
- Thyroid Neoplasm: Abnormal proliferative growth arising from thyroid tissue
- Hot nodule: Secretes thyroid hormones independent of TSH
- Cold nodule: Does not secrete thyroid hormones regardless of TSH; more likely malignant
Clinical Features
- Often asymptomatic
- Common presentation: palpable neck lump
- Later signs may include goitre and local compressive symptoms
Red Flags (Suspicious for Malignancy):
- Rapid growth
- Firm or hard consistency
- Fixed/immobile
- Hoarseness
- Dyspnoea
- Dysphagia
- Cervical lymphadenopathy
Green Flags (Reassuring Features):
- Mobile
- Painful
- Associated inflammation
Investigations
- Thyroid Function Tests (TFTs): Assess thyroid hormone production
- Ultrasound: First-line imaging for nodule characterisation
- Fine Needle Aspiration (FNA): Assess cellular atypia
- Radioisotope Scan: Identify “hot” vs “cold” nodules
- Histology: Post-surgical confirmation
Thyroid Adenoma – Follicular Adenoma (Benign)
- Prevalence: ≈90% of thyroid neoplasms
- Function: Can be hot or cold
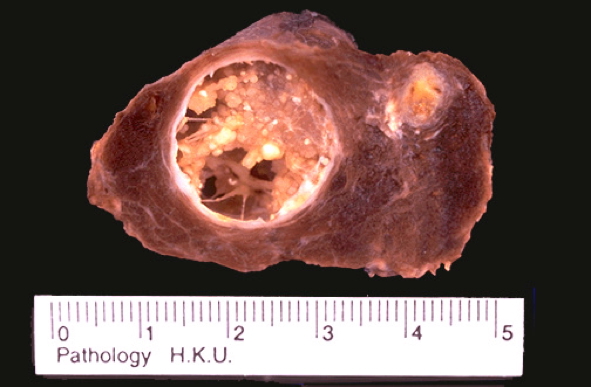
- Morphology:
- Solitary, spherical, encapsulated mass
- ~3 cm, well-circumscribed
- Cold = grey-white (↓colloid); Hot = red-brown (↑colloid)
- May show haemorrhage, fibrosis, calcification
- Clinical Features:
- Painless, unilateral mass
- Euthyroid (cold) or hyperthyroid (hot)
- Complications: No malignant potential; excellent post-surgical prognosis

Thyroid Carcinomas – Malignant Neoplasms (≈10%)
Papillary Carcinoma (Most Common)
- Origin: Follicular epithelial cells
- Presentation:
- Painless thyroid nodule
- Cervical lymphadenopathy often first sign
- Rarely compressive symptoms
- Treatment: Surgical excision
- Prognosis: Excellent – 98% 10-year survival
Follicular Carcinoma
- Origin: Follicular epithelial cells
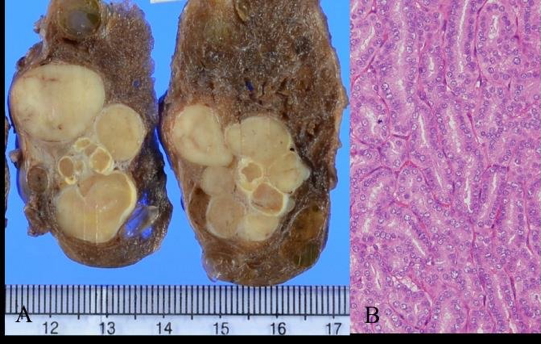
- Morphology:
- Single nodule, often with central fibrosis or calcification
- Can be well-demarcated or infiltrative
- Clinical Features:
- Slow-growing nodule
- Prefers haematogenous spread – often to bone
- No lymphadenopathy
- Treatment:
- Total thyroidectomy
- Radioiodine ablation
- Thyroid hormone replacement
- Prognosis: Moderately aggressive; metastases can present as pathological fractures
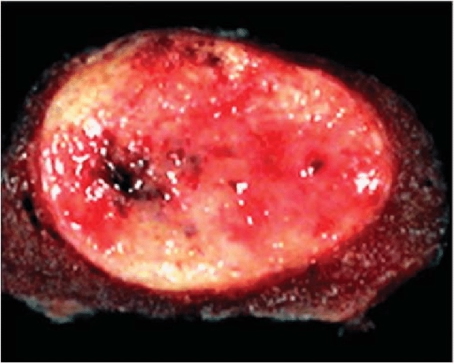
Anaplastic Carcinoma
- Pathogenesis: Arises from de-differentiation of papillary or follicular carcinoma
- Morphology: Aggressively invades local structures (e.g., trachea, vessels)
- Clinical Features:
- Rapid-growing neck mass in elderly
- Severe compressive symptoms
- Prognosis: Extremely poor – 100% mortality within 1 year
Medullary Carcinoma
- Origin: Parafollicular (C) cells of the thyroid
- Aetiology:
- 70% sporadic (RET proto-oncogene mutation)
- 30% familial (MEN 2A, 2B syndromes)
- Morphology:
- Solitary in sporadic; multiple in MEN syndromes
- Firm, pale with areas of necrosis/haemorrhage
- Can invade thyroid capsule
- Clinical Features:
- Thyroid nodule + dysphagia or hoarseness
- No hypocalcaemia despite high calcitonin
- MEN syndromes may include:
- Medullary thyroid carcinoma
- Phaeochromocytoma
- Parathyroid hyperplasia
Summary – Thyroid Neoplasms
Thyroid neoplasms include a spectrum from benign follicular adenomas to aggressive anaplastic carcinomas. Most are asymptomatic at presentation and require a structured approach to diagnosis using imaging, hormonal testing, and cytology. Prognosis varies greatly by subtype — from indolent papillary carcinoma to universally fatal anaplastic carcinoma. For a broader context, see our Endocrine Overview page.